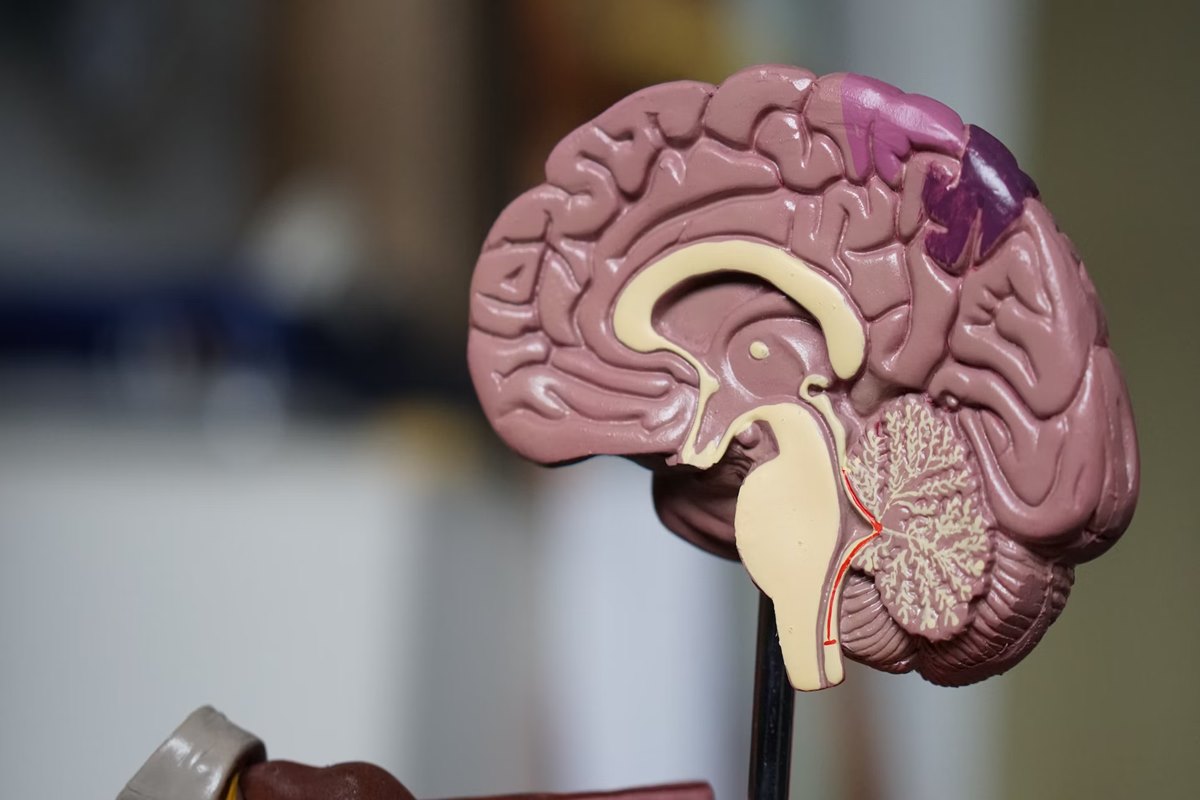
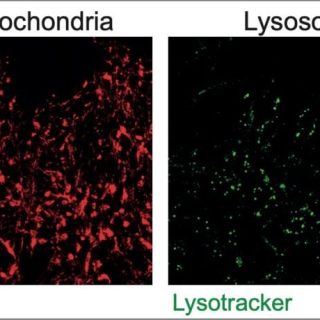
Parkinson’s disease is rife in this rural community, and some fear a toxic herbicide could be the cause

Scientists are concerned that a toxic herbicide widely used in Australian farming could be linked to the growing prevalence of Parkinson’s disease. It sat on the regulator’s shelf for review for decades, while the company manufacturing it worked to publicly discredit evidence that its product was harmful.
August 30, 2024