Ping-pong is not a game that lends itself well to chatter. It demands sharp focus, quick reflexes, and a light touch, and the dozen players who have gathered this Monday afternoon at PingPod, a table-tennis venue on West 99th Street, are locked in the wordless rhythms of the back-and-forth. Aside from the occasional “Nice spin!” or grunt of self-reproach, the room is filled with the hollow percussion of little white balls glancing off paddles, skipping over the tops of the black tables, and rattling across the floor.
Between games, one of the players, Lucy Miller ’81GS, praises the virtues of the activity. “Ping-pong is good for eye–hand coordination and coordination of the feet, so it’s good for people with Parkinson’s disease, because we have difficulty with those things,” Miller says. Like the other players here, Miller, who is seventy, is part of the New York chapter of a global organization called PingPongParkinson. Its members, all of whom have the disease, meet weekdays at ping-pong spots around Manhattan for community, exercise, and enjoyment. “It’s fun,” says Miller. “We have some pretty good players.”
Parkinson’s, or PD, is a progressive disorder in which brain cells involved in movement and coordination deteriorate and die. There are some ninety thousand new cases in the US each year, adding to the more than ten million cases worldwide, making it the world’s fastest-growing neurological disease. Celebrities like Michael J. Fox have raised awareness of Parkinson’s through their public struggles and advocacy, and in recent years such figures as Alan Alda, Linda Ronstadt, and Jesse Jackson have shared their diagnoses. Parkinson’s has also become the subject of legislation: this past summer, President Joe Biden signed the National Plan to End Parkinson’s Act, which will increase federal funding for related research.
The Parkinson’s Act is an important step forward in the effort to combat a disorder of profound mystery. Researchers don’t fully understand what causes it, and there is no cure. Men have double the risk of women, and adding to the puzzle is that no two cases are the same. The motor symptoms — tremor, slowness, muscle stiffness, trouble with balance and gait, and slow or slurred speech — vary from person to person. So does the rate of the progression. And while the disease is not in itself fatal, it can lead to life-threatening conditions.
A retired pharmaceutical researcher, Miller had been a promising ballerina as a teenager. But a knee injury changed that, and at twenty-one she enrolled at Columbia’s School of General Studies, where she majored in physiological psychology. About ten years ago, she began experiencing neurological issues, including speech problems. Doctors diagnosed her with Parkinson’s and prescribed levodopa (also known as L-dopa), which since the 1960s has been the standard treatment for tremor in Parkinson’s.
Hailed as a miracle drug, L-dopa is a precursor to dopamine, a neurotransmitter involved with movement. In Parkinson’s, different types of brain cells die, but it is the death of dopamine neurons specifically that causes the symptoms. L-dopa, taken in pill form, travels through the bloodstream into the brain, where it converts to dopamine. It also has a host of possible side effects, such as nausea, confusion, and, with long-term use, involuntary movements (dyskinesia).
“When I got the diagnosis, I was very upset,” Miller says. “But then, because I had so few side effects from the medication, I didn’t pay much attention to it.”
These days, Miller’s main concern is keeping her balance: Parkinson’s increases the risk of falls. That’s something Miller has to deal with each time she takes her spirited German shepherd puppy, Simone, for a walk. Ping-pong helps with balance, to be sure, but walking Simone can be an adventure, and Miller plans to get her trained.
Ever since the English physician James Parkinson, in his 1817 work An Essay on the Shaking Palsy, first unified the symptoms of tremor, stiffness, and altered gait into a single disease, scientists have battled to solve the riddles of Parkinson’s. For neuroscientist David Sulzer ’88GSAS, that quest borders on an obsession. Sulzer’s lab, located on Columbia’s medical campus in Washington Heights, focuses on how synapses — the junctions where two neurons meet and transfer information — are involved in neurodegenerative diseases such as Parkinson’s, Alzheimer’s, Huntington’s, and Lewy body dementia. “One of the problems with all these disorders is that they are only recognized at relatively late stages,” Sulzer says.
There are early, non-motor warning signs of Parkinson’s, such as constipation, depression, and trouble swallowing. Many people also experience loss of smell, lightheadedness after standing up, and REM sleep behavior disorder, in which they act out their dreams by kicking and thrashing. All these things may happen years before the telltale motor symptoms appear. In most cases, by the time of diagnosis, the brain has already lost 80 percent of its dopamine neurons.
Of the estimated hundred billion neurons in the human brain, only a tiny fraction — about four hundred thousand — make dopamine. Their axons — fiber-like structures that convey electrical impulses — are the longest of any type of neuron in the body. “If you stretch out one dopamine axon, it might be four meters long,” Sulzer says. “These neurons are very complicated, require a lot of energy and work to maintain themselves, and are susceptible to distress.” In Parkinson’s, that distress comes when alpha-synuclein, a protein that regulates the release of neurotransmitters, including dopamine, begins to misfold and accumulate within dopamine neurons, poisoning and eventually killing the cells.
Up until fairly recently, the hunt for the origins of the disease has focused on the brain’s movement centers. But over the past two decades, some scientists have turned their attention to another part of the body: the gut.
Sulzer is part of this “gut-first” movement, and he believes that Parkinson’s may have autoimmune features that start in the intestines. With a $9 million grant from the ASAP initiative (Aligning Science Across Parkinson’s, supported by Google cofounder Sergey Brin), Sulzer is leading a team of researchers from Columbia, the California Institute of Technology, the University of Alabama, and the La Jolla Institute for Immunology to get to the root of Parkinson’s. Working with Columbia neurologists Roy Alcalay ’10PH and Julian Agin-Liebes, neuropathologists Dritan Agalliu ’06GSAS and Osama Al Dalahmah, postdoc Francesca Garretti ’21GSAS, and graduate student Connor Monahan, the Sulzer Lab has been examining the role that gut neurons might play in the disease.
While the brain contains most of the body’s neurons, there are about one hundred million neurons in the gastrointestinal wall. In one experiment, the researchers injected mice with alpha-synuclein, which then gathered on the surface of the gut neurons. In response, the mice produced T cells — a type of white blood cell crucial for immune function — which attacked the affected neurons. The result? “The mice got gastrointestinal symptoms similar to those of Parkinson’s patients, including constipation,” Sulzer says.
Now Sulzer is working with immunologists who are examining the blood of people with Parkinson’s. “So far, we’ve been able to identify two proteins that are recognized by T cells of the immune system of Parkinson’s patients,” he says. “It’s even possible that this autoimmune attack is what’s causing the cell death in the disease.” The team published its findings this past summer in the journal Neuron. Sulzer’s goal is to develop a mouse model that fully mimics the human progression of the disease. If Parkinson’s actually starts in the gut, he says, it may be possible to identify and stop it before it reaches the brain.
Serge Przedborski, who is chief of the Division of Movement Disorders in Columbia’s neurology department, has spent years absorbed in another intriguing aspect of Parkinson’s: the uneven pattern of neuronal death. In Parkinson’s patients, he says, some brain cells are more susceptible than others to the disease process. As Przedborski explains, dopamine neurons are found primarily in two adjacent regions of the midbrain — the substantia nigra (SN) and the ventral tegmental area (VTA). But for some reason, it’s mainly the SN neurons that die. “These neurons have the same exact structure,” says Przedborski, “and yet even in advanced patients, you will always end with many more VTA neurons than SN neurons. Why?”
To find answers, Przedborski is using the tools of molecular and cellular biology. His lab focuses on the molecular basis of neurodegeneration, searching for the mechanisms in Parkinson’s by which cellular processes destroy one group of dopamine neurons but not the other. The brain has more non-neuronal cells than neurons, and some of these cells coexist with neurons and support them. Przedborski began to wonder what role these non-neuronal cells might play in neuronal health.
Working with immunologist Elizabeth Bradshaw, Przedborski and his team are using brain samples from the New York Brain Bank at Columbia to conduct a large-scale study comparing the features of neuronal and non-neuronal cells across different regions of the brain. Przedborski suspects that the non-neuronal cells, called glial cells, may influence neurons by creating environments that are either friendly or hostile. “We have shown that if you take a neuron which will eventually die from the disease process and put it in a more supportive environment, it will show greater resistance than the same neurons that you embed in a more hostile environment,” Przedborski says. “So if we can identify the molecular or cellular determinants that make the VTA neurons more resistant to Parkinson’s, we can try to devise therapies to boost the resilience of the more susceptible SN neurons. That’s the goal.”
The Sulzer Lab, too, is looking at VTA neurons. A decade ago, one of Sulzer’s postdocs, Yvonne Schmitz, using Parkinson’s model mice, discovered that the amino acid d-serine stimulates growth of dopamine neurons in the VTA. This causes the neurons to branch and extend into the depleted SN, where they supply enough dopamine to restore lost motor function — basically bolstering the work of L-dopa. Now Sulzer has received a grant from SPARKS NS, a nonprofit that funds promising clinical neuroscientific research. The researchers plan to do a small clinical trial on d-serine in humans. “This new approach, which we call ‘neurorestorative,’ may improve symptoms even after diagnosis,” says Sulzer, “and we hope it can help patients very soon.”
Columbia has been central to Parkinson’s research ever since neurologist Lewis Doshay founded the Parkinson’s Disease Clinic at Columbia in the 1940s. In 1957, William Black 1926SEAS, founder and president of Chock full o’Nuts, established the Parkinson’s Disease Foundation, the first private Parkinson’s philanthropic organization in the US (in 2016 it merged with the National Parkinson Foundation to become the Parkinson’s Foundation). Black also funded a building at Columbia, on 168th Street — the William Black Medical Research Building — which opened in 1965, with a floor dedicated to basic Parkinson’s science.
Doshay’s successor as clinic director was neurologist Melvin Yahr, whose studies of L-dopa in the 1960s led to its acceptance as the model treatment for motor symptoms in Parkinson’s. In 1967, Yahr and Columbia neurologist Margaret Hoehn created a system to grade the severity of Parkinson’s symptoms — the Hoehn and Yahr Scale, which is still used today. Yahr left Columbia to become chair of the neurology department at the Mount Sinai School of Medicine in 1973, and that’s when Stanley Fahn took over.
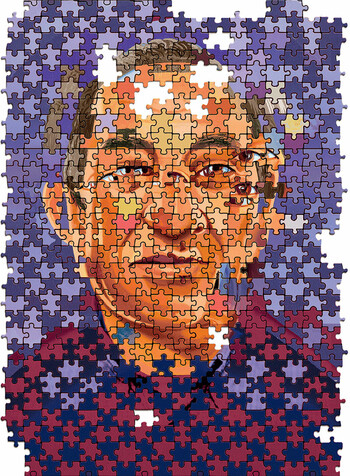
Fahn, now ninety-one and living in Westchester County, is a giant in the field. Sulzer calls him “the single most important member of the Columbia PD community” and “the most influential Parkinson’s neurologist after James Parkinson.” Fahn taught at Columbia for fifty-seven years and trained many of the world’s top Parkinson’s neurologists. In his work, Fahn determined that Parkinson’s was related to other, less common diseases that caused abnormal movements, such as Huntington’s disease, which is marked by excessive movement (hyperkinesis). To encompass the whole family of diseases, Fahn changed the name of the Parkinson’s Clinic to the Division of Movement Disorders and served as its director for forty years.
Today, Przedborski carries on the work of his predecessors, with technology undreamed of in Doshay’s day. In a current study, Przedborski, with Columbia neurosurgeon Gordon Baltuch and Weill Cornell neurosurgeon Michael Kaplitt, is investigating gene therapy for advanced Parkinson’s.
The idea is to program genes to instruct neurons to produce gamma-aminobutyric acid (GABA), a neurotransmitter that dampens hyperactive neuronal firing, thus mitigating the motor abnormalities of Parkinson’s. This is the principle behind deep brain stimulation (DBS), a mainstay surgical technique for people with severe motor disturbances. In DBS, doctors implant electrodes in the brain’s subthalamic nucleus (STN), a key structure in motor function, then stimulate it with electrical impulses. This basically jams the excessive neuronal activity of the STN that is a hallmark of Parkinson’s. Przedborski’s hope is that gene therapy will normalize motor circuits and improve symptoms without the need for the batteries and hardware used in DBS.
Baltuch is a pioneer of DBS and since the 1990s has performed thousands of operations. And yet he sees the motor symptoms of Parkinson’s as just part of the picture: a much harder problem for patients and caretakers, he says, comes at the end stages: cognitive decline. This occurs most frequently in people who have been diagnosed late in life. Overall, some 20 to 50 percent of people with Parkinson’s will develop problems with memory and attention, and about 80 percent of those cases will progress to full-blown dementia. “The holy grail of Parkinson’s is, How can we prevent cognitive decline?” Baltuch says. “Will we be able to use neuroprotective agents to prevent cells from dying?”
In theory, it’s possible. In practice, however, there is a serious impediment: the blood-brain barrier (BBB), a semipermeable membrane that protects the brain by filtering out harmful substances. While the molecules in some medications are small enough to pass through the BBB, the ones in the neuroprotective agents are too big. But as Baltuch notes, there is hope. This past year, Columbia biomedical engineers led by Elisa Konofagou and Sua Bae published a paper in the journal Theranostics detailing their success in using focused ultrasound waves in Alzheimer’s patients to safely permeate the BBB.
“If we can open up the BBB and then noninvasively inject neuroprotective agents to prevent cognitive decline and then close the BBB — that would be next-level,” Baltuch says. “Treating motor symptoms is obviously very important. But if the genie came out of the bottle and granted me one wish for Parkinson’s, I would immediately say: prevent cognitive decline. The rest we can deal with.”
“If the genie came out of the bottle and granted me one wish for Parkinson’s, I would immediately say: prevent cognitive decline.”
In 1997, Roger Duvoisin ’50CC, then chair of neurology at Rutgers Robert Wood Johnson Medical School, made a major discovery. He and his colleagues were studying the DNA of members of a large Italian family of six hundred people, more than sixty of whom had Parkinson’s. The team identified a shared gene mutation among the Parkinson’s carriers — the first to be implicated in the disease.
The gene, called SNCA, produces alpha-synuclein, that culprit protein that can misfold and accumulate within dopamine neurons. Duvoisin’s breakthrough opened a new frontier in Parkinson’s research. Since then, scientists have uncovered some twenty Parkinson’s-linked mutations that can be passed on genetically. These account for 10 to 15 percent of all Parkinson’s cases.
From the start, Columbia has been a leading center for the genetic study of Parkinson’s. Though the majority of cases are not tied to a genetic mutation, identifying and studying heritable mutations could illuminate the nature of the disease. Roy Alcalay and fellow Columbia neurologist Karen Marder have led studies showing that some populations have a greater likelihood of carrying a mutation: people with early-onset Parkinson’s (starting below age fifty); people with a strong family history of Parkinson’s; and people of specific ancestries. The most common mutations occur in the PRKN, LRRK2, and GBA genes, and studies at Columbia and elsewhere have found that Ashkenazi Jews and North African Berbers are more likely than other groups to carry the LRRK2 mutation.
The researchers also observed a correspondence between specific mutations and the ways different patients experience the disease. Says Alcalay, “We found that LRRK2 patients have a milder disease and less cognitive changes than those with the GBA mutation. People with GBA mutations have more non-motor symptoms, such as REM sleep behavior disorder and loss of sense of smell, have a faster disease progression, and are more likely to develop cognitive changes.”
These studies involved hundreds of people. Alcalay, recognizing the shortcomings of a blanket approach to treating Parkinson’s, saw the need to provide genetic data to a much larger population. If people with Parkinson’s knew their genetic status, he reasoned, they might opt to participate in trials for precision medicine, an approach increasingly used in oncology, in which doctors tailor treatment based on genotype and other individualized factors. Alcalay made his pitch, and in 2018 the Parkinson’s Foundation launched a nationwide genetic study, with Alcalay as its lead researcher.
This ongoing project, called PD GENEration, offers free genetic testing and counseling for people with Parkinson’s (genetic testing isn’t covered by health insurance). The study has expanded to all fifty states as well as the Dominican Republic, Mexico, Chile, Peru, Ecuador, Colombia, Israel, and Canada. To date, researchers have tested some eighteen thousand people, and more than 12 percent have turned up positive for a genetic mutation. That surprised Alcalay, who had expected roughly 5 percent. “As the study grows, more people may turn out to be positive, because science continues to identify new variants in known and novel genes,” he says.
To get the fullest, most useful genetic picture of Parkinson’s, it is vital to recruit people from as many backgrounds and parts of the world as possible. At Columbia, researchers are focusing on underrepresented people in the surrounding community, deploying Spanish-speaking research assistants and providing Spanish-language counseling. The math is simple, says Alcalay: “The more people who know their genotype, the more who will want to do clinical trials. And the more clinical trials that are done, the more likely they are to succeed — and the more likely we are to change the field.”
Recruitment is not easy. As Columbia neurologist Hiral Shah explains, some people may be suspicious of genetic testing, especially those belonging to groups with a history of mistreatment at the hands of the medical establishment. Shah, who works in the Division of Movement Disorders, focuses her research on Black and Latino populations in Harlem and Hamilton Heights, working with faith-based groups to spread awareness and strike down some of the myths around the disease (e.g., that it only strikes older white men, that symptoms like tremor or changes in posture or gait are part of normal aging, and that it’s contagious). “Until our health-care research is inclusive and represents our entire community,” says Shah, “we can’t expect to find the scientific results that are going to meaningfully change lives. We must bring everyone into the fold, because we believe that we could be one diverse patient away from a cure.”
Erika Adelman, who is the social worker for the Division of Movement Disorders and the social-work manager for the Neurological Institute at CUIMC, oversees many Parkinson’s programs, both in the community and at CUIMC, which offers a full range of patient resources. There is a patient support group and a caregivers’ support group. There is a virtual concert series, a speech-therapy collaboration with Teachers College, and a program called Parkinson’s Pals that connects patients to medical students in an attempt to reduce social isolation. There is a monthly access-to-care orientation that provides information on how to get home care, Medicaid accommodations, disability benefits, and transportation. And there is a program for those who have been diagnosed within the past nine months, in which neuropsychologists teach practical skills, coping strategies, and radical acceptance.
“People who get a Parkinson’s diagnosis often go through the stages of grief,” Adelman says. “And they go through this process at different rates. Radical acceptance means really learning to embrace the fact of the diagnosis and the fact that there’s a life beyond it.” As for managing the symptoms, Adelman encourages “exercise, exercise, exercise, because it is one of the best tools we have to fight back against this disease. We also recommend getting involved with meaningful social activities as well as doing brain-training
exercises like crossword puzzles, reading, or learning new instruments or languages, which increase the brain’s neuroplasticity. The brain is like a muscle — it needs to be worked.”
On another Monday afternoon at PingPongParkinson, Lucy Miller grabs a paddle. All around, balls skitter and hop. Miller happily reports that Simone, her German shepherd, has been through an intensive training course. Now, at Miller’s command, the dog will sit, stay, come, heel, and lie down. This will make their daily walks a lot easier.
At another table, Ron Hiram ’81BUS is in a groove. Hiram, seventy-one, spent years on Wall Street, then worked in venture capital. He was diagnosed with Parkinson’s in 2019, after his wife noticed his tremors. Hiram then began playing ping-pong and even hired a coach. He has a mean backhand and a nasty chop.
“For me, the major thing with PD is the tremor,” he says between serves. “I don’t take L-dopa — I’m a little fearful of the side effects — but eventually I don’t think I’ll have much of a choice.” Hiram walks at least three miles a day but says ping-pong is “the activity that makes me most motivated to exercise and do something for Parkinson’s.” He drops a serve and awaits the return.
At 3:30 p.m., the Monday session of PingPongParkinson ends. The players set down their paddles and retrieve their jackets and coats. It’s a strong community, self-governed and supportive. The game of life continues, and the players will be back next week.