Depression that appears later in life is often viewed as a response to declining health, but emerging evidence suggests it may sometimes signal deeper neurological changes.
Recent findings indicate that depression emerging later in life may reflect more than an emotional reaction to physical illness. Instead, it may signal the early stages of serious neurological conditions. A large nationwide study published in General Psychiatry offers the strongest long-term evidence so far, showing that depressive symptoms often appear years before a diagnosis of PD or LBD and can stay elevated well into the course of these diseases.
To explore this link, researchers analyzed extensive Danish national health records. They carried out a retrospective case–control study involving 17,711 people who were diagnosed with PD or LBD between 2007 and 2019. These individuals were matched by age and sex with people who had other long-term medical conditions, including rheumatoid arthritis, chronic kidney disease, and osteoporosis.
Depression Before and After Diagnosis
The analysis revealed a consistent trend. Depression was more common and appeared earlier in individuals who later developed Parkinson’s disease or Lewy body dementia compared with those diagnosed with other chronic illnesses.
As diagnosis approached, the likelihood of depression increased gradually and was highest during the three years immediately beforehand. Elevated rates of depression also persisted after diagnosis, remaining higher in patients with Parkinson’s disease or Lewy body dementia than in the comparison groups.
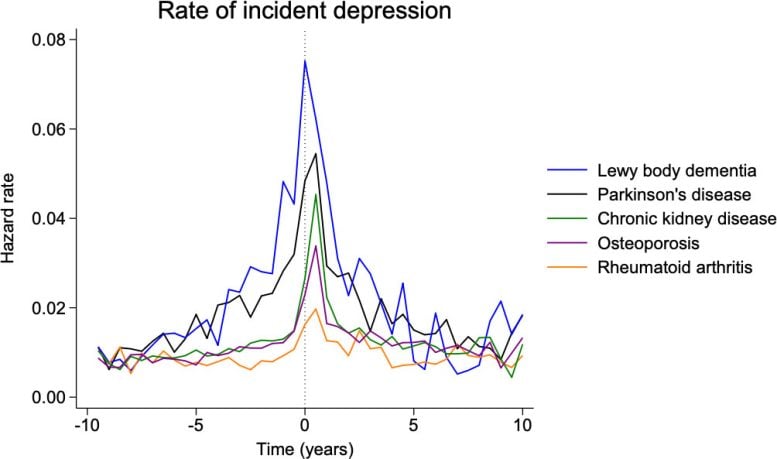
Notably, the observed rise in depression could not be attributed solely to the emotional challenges of managing a long-term medical condition. Other chronic illnesses that can cause significant physical limitations did not show a similar increase in depression rates. This pattern points to a possible connection between depression and early neurodegenerative processes in the brain, rather than depression being only a response to worsening physical health.
Differences Between Parkinson’s Disease and Lewy Body Dementia
The association was particularly pronounced in Lewy body dementia. Individuals with this condition experienced higher levels of depression than those with Parkinson’s disease, both before their diagnosis and in the years that followed. According to the researchers, variations in how these diseases progress and affect brain chemistry may help account for the difference.
“Following a diagnosis of PD or LBD, the persistent higher incidence of depression highlights the need for heightened clinical awareness and systematic screening for depressive symptoms in these patients.” first author Christopher Rohde noted “Thus, our main conclusion—that PD/LBD are associated with a marked excess depression risk preceding and following diagnosis when compared with other chronic conditions—remains valid.”
The authors emphasize that this does not mean everyone with depression will develop Parkinson’s disease or dementia. Instead, they recommend greater awareness and closer monitoring when depression appears for the first time in older adults.
While there is currently no cure for Parkinson’s disease or Lewy body dementia, addressing depression early could improve quality of life and overall care for patients as these diseases develop.
Reference: “Depression preceding and following the diagnosis of Parkinson’s disease and Lewy body dementia” by Christopher Rohde, Martin Langeskov-Christensen, Lene Bastrup Jørgensen, Per Borghammer and Søren Dinesen Østergaard, 3 December 2025, General Psychiatry.
DOI: 10.1136/gpsych-2025-102405
Never miss a breakthrough: Join the SciTechDaily newsletter.
Follow us on Google and Google News.