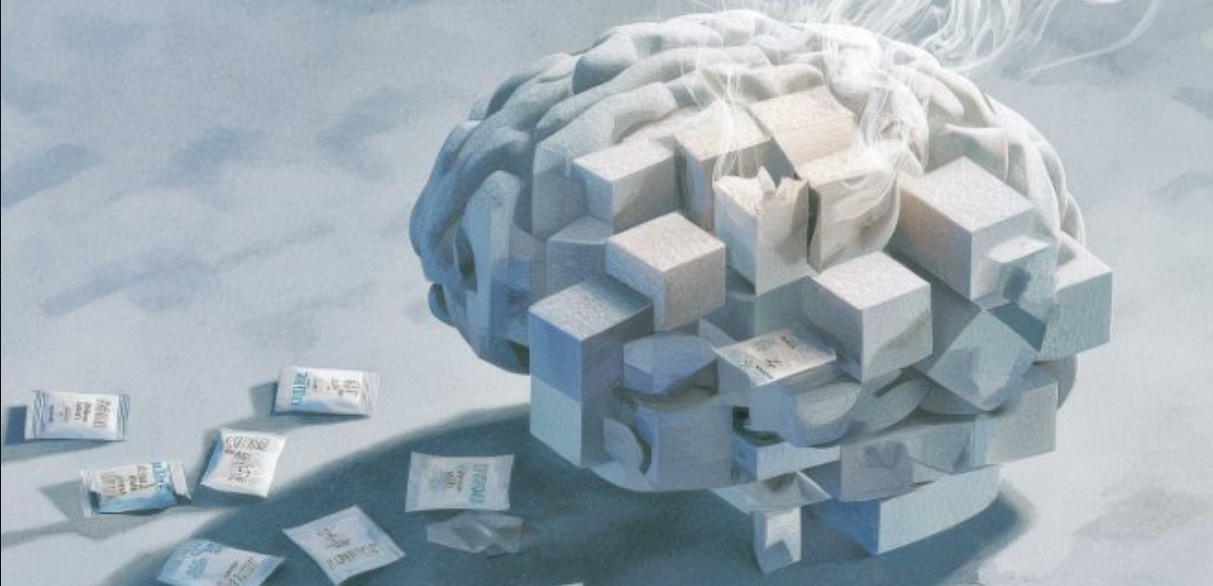
Depression that arises later in life is often dismissed as a normal response to ageing or health challenges. However, emerging evidence suggests it may sometimes indicate underlying neurological changes rather than simply reflecting emotional strain.
A study published in General Psychiatry highlights that depression appearing in older adults could be an early warning sign of neurodegenerative diseases, such as Parkinson’s disease (PD) and Lewy body dementia (LBD).
More To Read
The research found that depressive symptoms often emerge years before a formal diagnosis, suggesting that late-onset depression may serve as an early marker of brain changes.
People who later developed PD or LBD showed higher rates of depression than those diagnosed with other chronic illnesses, including rheumatoid arthritis, chronic kidney disease, or osteoporosis. This demonstrates that the increase in depression is not merely a reaction to living with a long-term medical condition.
Understanding the conditions
• Parkinson’s disease: A progressive brain disorder affecting movement, causing tremors, stiffness, slow motion, and balance problems, often accompanied by depression and cognitive changes.
• Dementia: A decline in memory, thinking, and daily functioning, commonly caused by conditions like Alzheimer’s disease or LBD.
The study revealed that depression gradually increased in the years leading up to a PD or LBD diagnosis, peaking in the three years immediately before diagnosis. Elevated depression levels also persisted after diagnosis, remaining higher than in patients with other chronic diseases.
The link between depression and neurodegeneration was particularly strong in individuals with Lewy body dementia. These patients experienced more pronounced depression than those with Parkinson’s, both before and after diagnosis—a difference likely tied to variations in disease progression and brain chemistry.
“Following a diagnosis of PD or LBD, the persistent higher incidence of depression highlights the need for heightened clinical awareness and systematic screening for depressive symptoms in these patients,” said first author Christopher Rohde.
“Our main conclusion—that PD and LBD are associated with a marked excess depression risk preceding and following diagnosis compared with other chronic conditions—remains valid.”
Implications for care
While not all older adults with late-onset depression will develop PD or LBD, the study underscores the importance of careful monitoring and early intervention.
Detecting depression early in older adults could improve quality of life and help provide better overall care as neurodegenerative conditions progress.
Researchers analysed Danish national health records in a retrospective case–control study involving 17,711 individuals diagnosed with PD or LBD between 2007 and 2019. Each participant was matched by age and sex with people suffering from other long-term conditions.
Other Topics To Read
The findings showed that depression was more common and appeared earlier in those who later developed PD or LBD, confirming a potential link between late-onset depression and early neurodegeneration rather than a simple response to declining physical health.

