Imagine struggling with a common sleep issue, and next thing you know, you might be at risk of developing Parkinson’s disease.That’s right — a large new study reports a link between obstructive sleep apnea (OSA) and a higher chance of developing Parkinson’s disease years later. The research — using millions of electronic health records — found people with untreated OSA were more likely to receive a Parkinson’s diagnosis. At the same time, those who began CPAP therapy early had a lower risk.
What does the study say
The major new study, published in JAMA Neurology, analyzed more than 11 million medical records of US veterans over more than two decades, and found that individuals with untreated OSA (obstructive sleep apnea) had a significantly higher risk of developing Parkinson’s disease compared to those without OSA.Researchers observed that those who never received effective treatment for OSA were nearly twice as likely to be diagnosed with Parkinson’s over time.

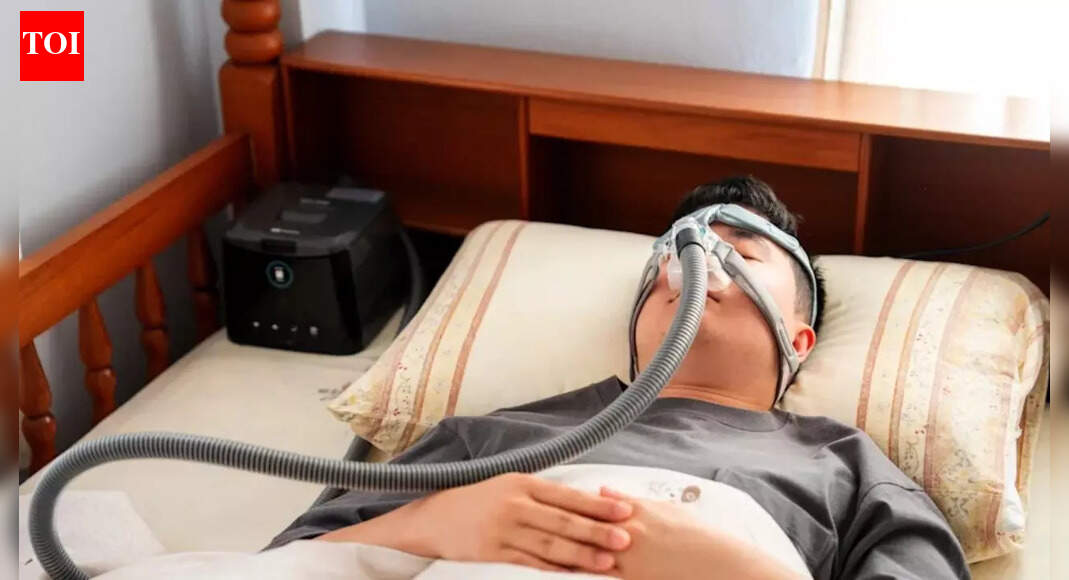
Crucially, the study also tracked people who received treatment early, specifically with a Continuous Positive Airway Pressure (CPAP) machine, and quite notably, participants who started CPAP therapy within about two years of their sleep-apnea diagnosis showed a significantly lower incidence of Parkinson’s compared with untreated individuals.It’s important to note that the study doesn’t prove that OSA causes Parkinson’s. However, the strength of the association — even after accounting for factors like age, obesity, or cardiovascular disease — makes it hard to ignore.
What is obstructive sleep apnea (OSA)?
Obstructive sleep apnea (OSA) is a condition where the airway gets blocked repeatedly during sleep, causing you to stop and start breathing. It happens because the muscles in the back of the throat relax too much, leading to an airway collapse that causes loud snoring, gasping, or choking, and brief awakenings that prevent restful sleep.
What is Parkinson’s disease?
Parkinson’s disease is a progressive nervous system disorder that causes problems with movement, such as tremor, stiffness, and slowness. It is caused by the loss of nerve cells in the brain that produce dopamine, a chemical crucial for smooth, controlled movement. Symptoms of this neurogenerative disorder often begin on one side of the body and worsen over time, potentially affecting balance and coordination, walking, and talking.
Why might sleep apnea lead to neurodegeneration
As per the study, experts think the link may come down to chronic oxygen deprivation and disrupted brain restoration during sleep. In OSA, breathing repeatedly stops and starts during sleep, causing drops in blood oxygen and frequent awakenings. Over time, this repeated lack of oxygen (hypoxia) and sleep fragmentation may impair the brain’s ability to “cleanse” itself.

One recent study pointed toward dysfunction of the Glymphatic system, which is the brain’s waste-clearance system, in people with sleep apnea. When glymphatic function is impaired, toxic proteins may build up, possibly contributing to neurodegenerative diseases such as Parkinson’s. So, in other words, poor sleep isn’t only the starting point of health hazards like exhaustion and cardiovascular strain — it may gradually starve neurons of oxygen, disrupt repair and waste-removal processes, and raise vulnerability to long-term nerve damage.
What you should do
Early diagnosis of sleep apnea: Firstly, recognizing symptoms such as loud snoring, gasping for air during sleep, frequent awakenings, morning headaches, or excessive daytime drowsiness, and consulting a specialist, is crucial, as that enables you to take the next step toward resolving the health hazard. A formal sleep study can diagnose OSA. Because oxygen drops and disrupted breathing are often the culprits behind long-term risks, timely diagnosis matters.Use of CPAP (or other recommended treatments): If diagnosed with OSA, using CPAP — which keeps the airway open during sleep — appears to significantly reduce the risk of Parkinson’s, according to the study. Starting CPAP treatment early — ideally within two years of OSA diagnosis — seems particularly important for risk reduction.Improvement of sleep hygiene and lifestyle: Besides CPAP, there are other supportive steps that help as well. For example, maintain a regular sleep schedule and ensure a sleep-friendly environment — a cool, dark room with minimal disturbances. Avoid alcohol or heavy meals close to bedtime (as they worsen airway obstruction). Additionally, maintain a healthy weight and exercise regularly, as obesity and poor metabolic health often worsen OSA.Monitor brain and sleep health, especially in midlife: If you have OSA or experience changes in sleep quality, periodic follow-up with a neurologist or sleep specialist can help catch early signs of neurodegeneration.