I always looked up to John Stapleton and, during my stint as a “TV doc” during the Nineties, did everything I could to emulate his calm but incisive presentation. I never quite managed it but I did meet him a couple of times and, unlike some heroes, he didn’t disappoint. So I was saddened to hear of his death at the weekend, less than a year after he announced that he had Parkinson’s.
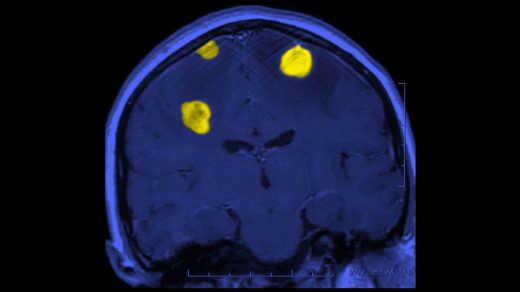
One in 37 of us are predicted to develop Parkinson’s at some stage and, while it does shorten life expectancy, many will live with the condition for years and sometimes even decades. It is caused by progressive degeneration of dopamine-producing nerve cells in the substantia nigra, a small part of the midbrain that, among other things, helps to control movement and muscle tone.
Why some people develop Parkinson’s and others don’t remains unclear but, as with many diseases, it is thought to be a combination of genetic predisposition and environmental factors. Men are at slightly higher risk than women, as are some people with a family history of Parkinson’s, but there is still much debate as to which environmental triggers — anything from viral infection to pollutants — might be responsible.
• Read more expert advice on healthy living, fitness and wellbeing
At the moment treatment is aimed at boosting dopamine function in the brain with drugs such as levodopa, along with exercise and physio, speech, language and occupational therapy. However, while these improve symptoms and quality of life, they don’t stop the inexorable progression of the disease — the real game-changer will be new therapies that slow, or even reverse, the underlying degenerative changes.
There are lots of these new disease-modifying drugs in the pipeline but, even if they work as hoped, for maximum benefit they will need to be given much earlier in the course of the disease than present treatments. Early diagnosis will be much more important than it is now, as by the time most cases are confirmed, much of the damage has already been done.
Typically the diagnosis isn’t made until the individual — or their friends, family or doctor — notices the classic telltale signs such as tremor (see below), a slow, shuffling or unsteady gait and a blank, expressionless face. As Stapleton revealed in his last interview with The Sunday Times: “My mother had Parkinson’s so I knew the signs. I had a tremor, difficulty swallowing — my voice changed. And I was beginning to walk with the Joe Biden shuffle.” Albeit in Biden’s case, that is not confirmed as due to Parkinson’s.
Present treatments can have a dramatic impact but maintaining this benefit is often difficult. New disease-modifying treatments may change that but, however effective they prove, the earlier they are started, the better the prognosis is likely to be. So can we catch it sooner?
We now know that the classic symptoms are preceded by others, sometimes up to a decade earlier. These include an impaired sense of smell, constipation and frequent vivid and/or aggressive dreams (REM sleep disorder). However, these are all common and can be caused by all sorts of far less worrying factors, ranging from allergies or Covid (smell), to side-effects of medication, stress or anxiety. That is why researchers are working hard to identify more reliable tests.
One example is a blood test that identifies eight different markers (proteins) in the blood associated with Parkinson’s. In early testing by a team from University College London it has proved very accurate at predicting who will go on to develop clinically obvious disease, and up to seven years before classic symptoms like tremor develop.
• £80 blood test could detect Parkinson’s disease before symptoms
Elsewhere researchers supported by Parkinson’s UK are testing a new drug — PXS-4728 — on people with REM sleep disorder to see if it can delay the development of Parkinson’s or prevent it altogether.
All of which, while exciting, will be of little consolation to families like the Stapletons. And there are many of them, with latest estimates suggesting that there are nearly 170,000 people living with Parkinson’s in the UK.
On the upside, thanks to existing treatments most people with Parkinson’s continue to have fulfilling lives for many years, but the prognosis is variable depending on the individual, their age and their general state of health. Those diagnosed at a younger age, such as the actor Michael J Fox, tend to fare better, but there are always challenges, with complications including bladder and bowel problems, pneumonia (often caused by swallowing difficulties), depression and dementia, as well as the obvious mobility issues.
However, a UK study quoted by the National Institute for Health and Care Excellence in its latest guidance on Parkinson’s found that, ten years on from their diagnosis, a quarter of people with the condition still had the same level of mobility and cognitive function. A proportion that will increase dramatically if just a few of the medicines in the pipeline prove effective.
Parkinson’s: the facts
• Parkinson’s is mostly seen in older people but can develop earlier in life. About 1 in 20,000 people in their thirties in the UK have the condition, compared with about 1 in 60 of those in their early eighties.
• Tremor is common in older people and often not related to Parkinson’s but it is one of the classic symptoms. In Parkinson’s the tremor/shaking is characteristically worse at rest (with your hand on your lap) and less obvious on movement (when you pick things up).
• While GPs like me can diagnose Parkinson’s it should always be confirmed by a specialist team, who can also tailor treatment to the individual’s needs.
• For more information on diagnosis and treatment visit parkinsons.org.uk