Farmers’ warning over paraquat chemical’s link to Parkinson’s Disease

John O’Brien was diagnosed with Parkinson’s Disease three years ago. (ABC Central West: Hamish Cole)
As a child, John O’Brien would spend hours in the paddock helping his dad spray crops to protect them from weeds and pests.
Now as a 68-year-old, he believes those same chemicals he used — like the broad-spectrum herbicide paraquat — may be behind his Parkinson’s Disease diagnosis.
He is not alone.
In his tiny district, five other farmers told the ABC they have been diagnosed with the disease and take medication two or three times a day.
They all live within 10 kilometres of Mr O’Brien.
None of the farmers are related but all have grown up in Crookwell, on the New South Wales southern tablelands, and all of them have used paraquat throughout their farming life.
Mr O’Brien said he would regularly be immersed in paraquat while spraying his potato crops, which he did every two months for years.
“You had the boom spray in front of the tractor, no cab … it would be blowing the chemical up on your face all the time,” he said.
“When you were spraying the spuds and all that, you would be covered in it.”
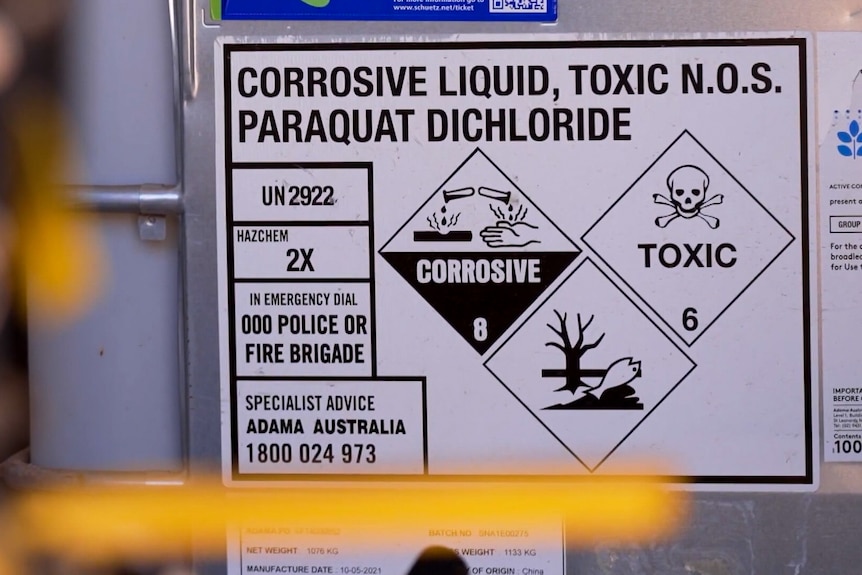
The use of paraquat in Australia is currently under review by the Australian Pesticides and Veterinary Medicines Authority. (Supplied)
The ABC uncovered the farmers through a crowdsource investigation following a Landline report that investigated the links between paraquat and the neurological disease.
Parkinson’s Disease is an incurable neurodegenerative brain condition that causes problems with movement, mental health, sleep and cognitive function.
More than 150,000 Australians are believed to be living with Parkinson’s.
It is the fastest growing neurological disorder in the world.
According to the World Health Organization there is no known cause of the disease, however exposure to pesticides may increase the risk.

Mr O’Brien experiences common symptoms of Parkinson’s Disease such as muscle aches and shaking. (ABC Central West: Hamish Cole )
The use of paraquat in Australia is under review by the Australian Pesticides and Veterinary Medicines Authority (APVMA).
The APVMA said it would not comment while its regulatory review was underway, but previously told the ABC it “considers scientific information from a variety of sources when reviewing agvet chemicals to determine their safety”.
The regulator has found the evidence linking paraquat with Parkinson’s was “not robust”.
The APVMA has also made changes to the product label and personal protective equipment (PPE) requirements, and said if used according to guidelines — which are now stricter than ever — it does not believe paraquat is unsafe.
The company who first made paraquat, Syngenta, said there was no proof the chemical caused Parkinson’s Disease and maintained the product was safe for farmers to use.
Grain growers also argue the herbicide is vital to crop production and say a ban could severely impact food supply and sustainable farming practices.
Childhood innocence
Jane was also brought up on a farm in the Crookwell district, at the same time as Mr O’Brien.
She was diagnosed with Parkinson’s more than a decade ago.
Jane’s real name has been withheld to protect her identity and because she does not want her diagnosis to be public.

Crookwell is a small town located about 100km north of Canberra. (ABC Central West: Hamish Cole)
On her family’s potato farm, Jane and the other kids would collect the crop after it had been sprayed with paraquat.
Small fires were often lit to burn off the vegetation left behind from the potatoes.
“We would throw the potatoes into those fires to let them get really charred and then eat them, no washing or anything like that,” she said.
“I am coming to the realisation now that a lot of that innocence of childhood would have had a big impact on my overall health.”
Growing evidence of a link
Neuroscience Research Australia chair Professor Carolyn Sue said paraquat was increasingly being linked to Parkinson’s.
“There is growing evidence that this chemical in the environment can cause Parkinson’s Disease,” she said.
“We know that farmers for example, in rural areas who use pesticides, herbicides, can have an increased risk of having Parkinson’s in their life span.”

Professor Sue says there is a growing link between pesticide exposure and Parkinson’s Disease. (Supplied: Neuroscience Research Australia)
Experiments exposing animals to chemicals used in pesticides have led to cell changes in the brain that replicate the symptoms of Parkinson’s in humans.
“Animal studies certainly have shown a causative link,” Professor Sue said.
“They have actually caused changes that are consistent with Parkinson’s Disease in those animals, the type of nerve cells that are affected and the symptoms are very similar.”
As someone who treats Parkinson’s patients, Professor Sue believes people should avoid contact with the chemicals at all cost.
“As health providers to patients who are affected with Parkinson’s Disease, one would think about trying to reduce exposure to such agents,” she said.
Wondering ‘Why me?’
Jane was diagnosed in 2013 after beginning to display symptoms of Parkinson’s such as tremors in her hands.
“It just got to the stage where it was becoming socially unacceptable … as soon as the anxiety kicked in, the shakes got worse,” she said.
“I do sort of wonder sometimes ‘Why me?’ But maybe looking back on my childhood some of the things maybe I shouldn’t have done or someone should have prevented me from doing.
“That is hard to take now.”

Mr O’Brien says he was regularly exposed to paraquat while working on the family farm. (ABC Central West: Hamish Cole)
Mr O’Brien was diagnosed three years ago after displaying similar symptoms.
“I am a person who takes each day as it comes,” he said.
“I just took it in my stride and tried to make sure that I could keep doing the things that I was doing instead of getting me off the farm.”
Support service under-funded
Parkinson’s New South Wales is the peak body for assisting patients, and currently receives $33,000 annually from the state government, and no funding from the Commonwealth.
“That equates to 47 cents per person with Parkinson’s and that is what we have got to be there for people when they get diagnosed,” chief executive Mary Kay Walker said.
“We are there for people with Parkinson’s every step of the way, from their diagnosis to the end stages … we do it with 97 per cent of our funding coming from donations and fundraising.”
NSW Health Minister Ryan Park said Parkinson’s NSW had received an additional $800,000 in “ad-hoc grant funding” since 2021.
Mr Park said $8.6 million was also set aside over a four year period to fund nursing and allied health staff to support people with movement disorders, such as Parkinson’s.
“Patients with Parkinson’s and other movement disorders receive a range of health care services including specialist neurology services, and nursing and allied healthcare support to help manage their condition and promote independence and wellbeing,” he said in a statement.
“Many people with Parkinson’s Disease require support with functional impairment and may be eligible for NDIS or aged supports.”
The federal health department has been contacted for comment.
For Mr O’Brien, he hopes sharing his experience will help bring about more support for other people diagnosed with the condition.
“If I can shorten the period where they find a cure for Parkinson’s by one day I will be happy,” he said.
“I want to see something that will help people with it, like myself, that will stop the pain, the spasms, that symptoms that we have that are caused by Parkinson’s.”
Loading…