Abstract
Understanding what matters to people with Parkinson’s and their family is essential to derive relevant clinical outcome measures and guide clinical care. The purpose of this study was to explore what is important to people with Parkinson’s disease vs. family over time. A qualitative content-analysis of online survey data collected by Parkinson’s UK was conducted to identify types and frequencies of important symptoms and impacts of Parkinson’s for people with the disease vs. family of people with Parkinson’s. Independent T-tests were used to identify significance of between group differences for patients vs. family at < 2, 2–5, 6–10, 11–20, > 20-year durations. ANOVA was used to assess for within group differences by disease duration. We found that symptom priority changed significantly over time with longer disease duration. Tremor was reported less often later on, whereas mobility, dyskinesias, gait and speech/communication symptoms gained priority. In general, patients identified movement-related symptoms (e.g., walking, bradykinesia) as the most bothersome at all durations while family more strongly prioritized the physical and psychosocial impacts of disease (e.g., mobility, safety, interpersonal interactions, independence, and family impact). We conclude that important differences exist between family and patient perspectives of what matters and change over time with longer duration of disease.
Introduction
Understanding what is meaningful to patients is essential to developing relevant clinical outcome measures that can be used in clinical trials to test the efficacy of new therapies1. Recent studies have helped to increase understanding of what is meaningful to people with Parkinson’s disease (PwP)2,3,4. However, further evidence is needed in support of these findings, along with greater specificity on health experiences and rationales for why certain aspects are most bothersome. This type of granular data is needed to develop regulatory-approved, patient-centric measures, which can be used to assess if new treatments lead to clinically and personally relevant change in disease outcomes5, and to support patient-centric clinical care.
Regulatory agencies have identified patient focused drug development as a high priority for clinical trials in the Patient-Focused Drug Development (PFDD) guidance series, which delineates expectations for collecting data on meaningful aspects of health5. The PFDD series was developed to ensure that patients’ “experiences, perspectives, needs, and priorities” are adequately represented and reflected in drug development and evaluation, and that novel therapies prioritize what matters to people with lived experience (e.g., patients and care-partners)6. With a growing number of promising therapies in the pipeline for PD, there is an urgent need to assure that outcome measures for clinical trials align with regulatory expectations and the needs of the patient community7. Data are also needed to understand whether what is important to the individual with PD corresponds with what is important to their loved ones, who are also deeply affected by disease processes8,9,10. This is not only important for family-oriented care in clinical practice, but for development and validation of clinical outcomes measures, which are needed to measure the efficacy of new drugs to delay or halt disease progression5. Thus, the purpose of this study was to explore what affected individuals consider the most important aspects of Parkinson’s disease (PD) and compare what is important to People with Parkinson’s disease (PwP) versus family members at different durations of disease.
Methods
Study background, setting, & sample
This study is a qualitative analysis of anonymous online survey data collected by Parkinson’s UK in 2018 to identify which symptoms of PD were perceived as most important to people affected by PD4. PwP and their family (defined as spouse, partner/significant other, child of PwP) were recruited from the Parkinson’s UK network email distribution lists (N ~ 4800 members). Participants had given prior consent to correspondence with the foundation for research purposes. The study was deemed written consent exempt; all data were submitted anonymously, and all respondents agreed to a disclosure statement. IRB approval was obtained for data analysis from University of Massachusetts, Dartmouth (IRB#23.056) and was conducted in accordance with the declaration of Helsinki11.
Data collection
The online survey was developed by Parkinson’s UK and a 6-member PwP advisory panel. The survey was designed to be low-burden and took about 5 min to complete. A prequel to the survey stated the purpose and disclosures. Those who agreed to participate were asked basic information about their role (PwP or family of PwP), the age of the PwP, and duration of PD (years since diagnosis). Next, each respondent was asked the following questions on a single page, all of which were free response items with unlimited response length.
- 1.
What particular aspects of your Parkinson’s would, if improved, make the biggest difference to your life? These could be movement or non-movement symptoms or could be side effects related to your Parkinson’s treatment. Please list up to three in the [three] boxes below with the most important first.
- 2.
Please tell us why you chose these.
No additional prompts were provided, and participants could answer questions in whatever manner they chose.
Data analysis
Qualitative coding
Data were extracted to an Excel file, and qualitative content coding was used to systematically code each entry for all aspects that respondents reported as meaningful. Data were coded by a first coder (MT) who used open coding to develop a list of all mentioned factors and systematically coded each case for presence/absence of each item. A case was defined as all three entries with supporting explanations from a single participant. All coding was validated by a second coder (JM).
Concepts were coded as 1 = first priority, 2 = second priority, 3 = third priority, and 4 = rationales and further details on what made the experiences important. Due to the open response format, respondents were able to report multiple important factors within a single response box. These included symptoms, impacts, and contextual factors. Thus, a single individual could have unlimited factors coded as important aspects of their PD experience. After initial content coding, redundant or conceptually duplicate items were merged. Related codes were clustered using domain groupings from the Consensus Conceptual Model in early PD (e.g., movement, cognitive, psychiatric, sensory, sleep, speech, digestive, urinary, sexual, autonomic, physical function, psychosocial functioning)12.
Statistical analysis
After curation by domain, frequencies of important factors were derived for each PD duration grouping (< 2 year, 2–5 years, 6–10 years, 11–20 years, > 20 years with PD) with comparison between duration-matched PwP and family groups to identify between group differences at each stage. Descriptive statistics were computed for survey items. Frequencies were computed for all factors reported as important aspects of the PD experience identified as 1st, 2nd, 3rd priority or rationales. Spearman’s r effect size for Chi-square test of independence was calculated to assess association between what is important and PwP age, with a negligible relationship considered 0.10 or less, a weak relationship as > 0.10 to 0.29, moderate relationship as 0.30–0.39, strong relationship > 0.4, and very strong relationship > 0.713. Next, independent T-tests were used to identify significant between group differences for PwP vs. family at < 2, 2–5, 6–10, 11–20, > 20-year durations. For T-tests, important factors analyzed as either present or not present. ANOVA was used to assess for within group differences by disease duration (e.g., PwP at < 2, 2–5, 6–10, 11–20, vs. > 20 years duration; family at < 2, 2–5, 6–10, 11–20, vs. > 20 years duration). Survey responses that did not identify the PwP’s age (n = 12) were removed from subgroup analyses.
Measures to enhance validity
Measures to enhance validity include use of two PhD-prepared qualitative researchers (JM, MT) during coding and coding validation, participant numeric identifiers for quotations, Standards for Reporting in Qualitative Research14 and inclusion of coded data in Supplemental materials.
Ethics approval
IRB approval was obtained from University of Massachusetts, Dartmouth (IRB#23.056).
Informed consent
Data in this study were collected anonymously via survey, with no identifiers and no potential risks. Therefore, this study was given exempt status in compliance with federal exemption categories §46.104 Exempt Research Category 2, and written informed consent was not required or obtained per federal regulations: https://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/common-rule-subpart-a-46104/index.html. Instead, participants gave general written consent to correspondence with Parkinson’s UK for research purposes.
Results
Sample characteristics
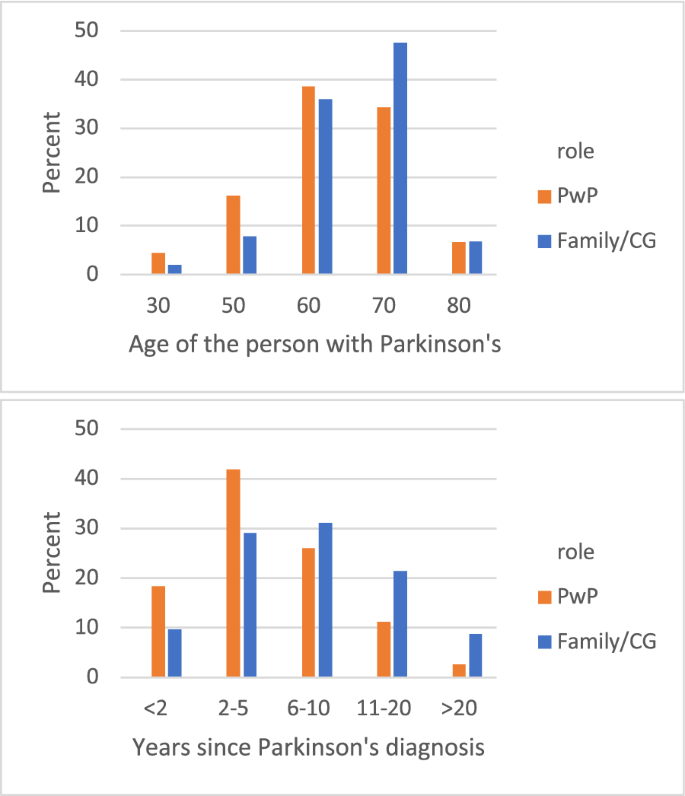
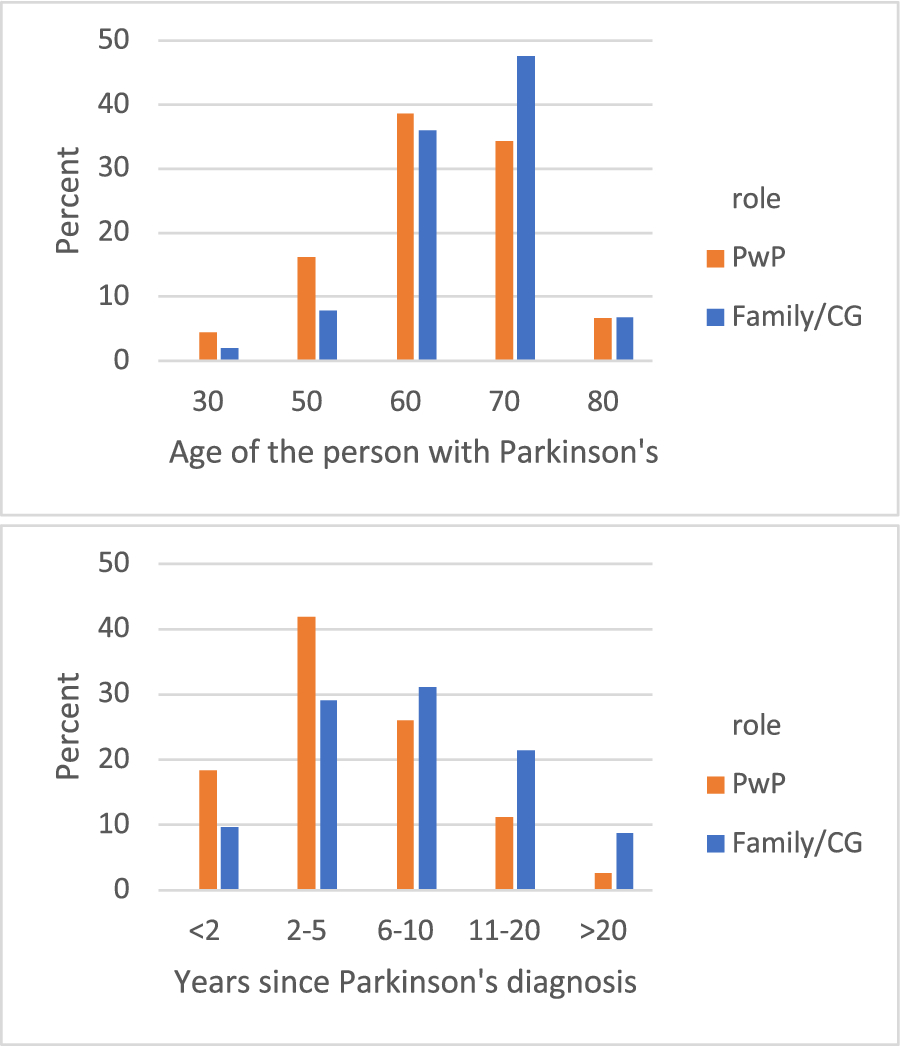
In all, 823 participants responded to the online survey. After excluding responses of unknown PD duration (n = 43; 5%) a total of 780 unique participant responses were included in the analyses. Sample distribution was 677 PwP (82.3%) and 103 family of PwP (12.5%). More than half of those sampled (54.3%) were within 5 years of PD diagnosis, with PwP aged 50–70 years old (84.5%). Demographics of the population were 92% white, 52% female, < 44% college-educated, and 40% urban/suburban. As shown in Fig. 1, there was a significant difference in PwP age and years since diagnosis between the family vs. PwP group. In general, family respondents reported experiences about PwP who were older and further from diagnosis (p = 0.008, p ≤ 0.001, respectively).
Correlations of important factors with PwP age
As shown in eTable 1, negligible to weak-significant correlations existed between age and many common movement symptoms such as bradykinesia, difficulty with walking & balance, dystonia, and restless legs. This was also true for age and many non-movement symptoms, such as multitasking ability, pain, changes in speech, and urinary symptoms, as well as functional impacts of decreased ability to self-care, trouble eating, safety issues, decreased independence, and loss of pleasurable activities. There were no moderate or strong correlations between age and frequency of any factors.
Most important aspects of PD
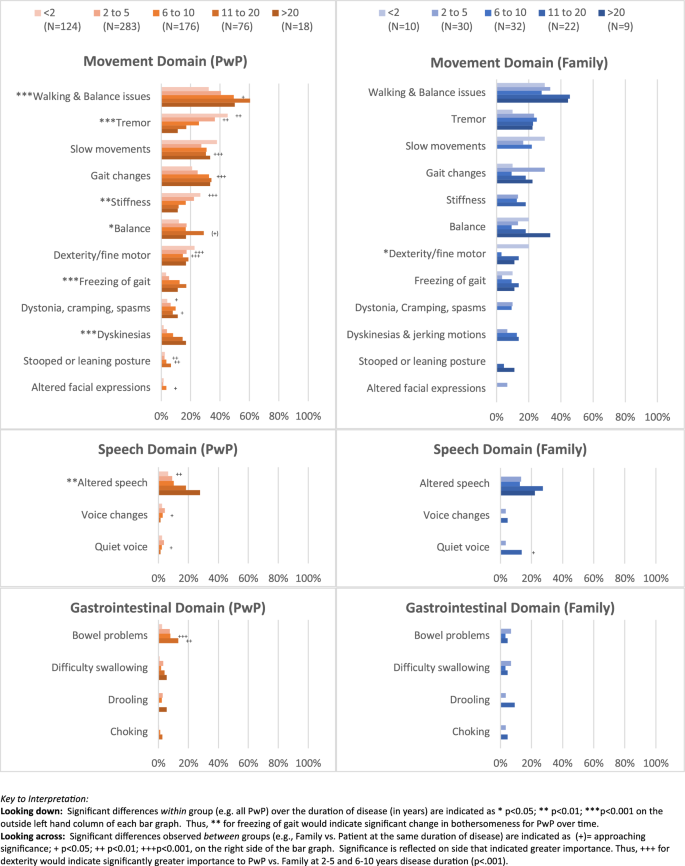
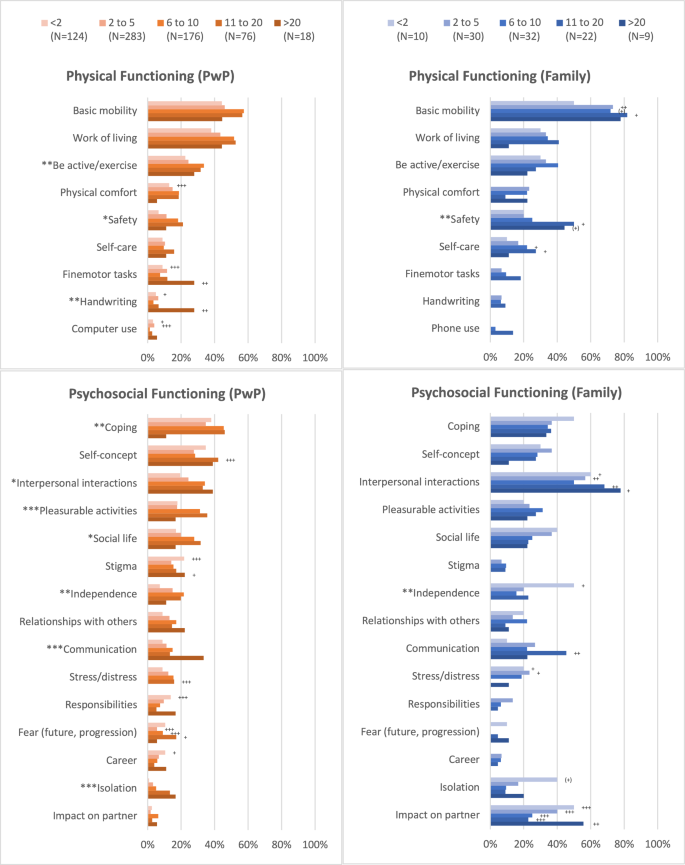
PwP and family reported over 200 unique factors as important aspects of the Parkinson’s disease experience. Most important aspects included a wide range of symptoms, impacts on physical and psychosocial functioning, and contextual issues relating to PD management. Side-by-side comparisons of the most common factors are presented graphically in Fig. 2a–d with frequencies and statistical significance of within group (over time) and between group differences (PwP vs. family) for all reported factors in eTable 1.
Most important aspects of PD reported by PwP
Movement-related symptoms were most pervasively bothersome to PwP at all durations of disease, and were cited by 83% of the total PwP sample, increasing from 81% in early PD to 94% in late PD. Tremor was most bothersome early on (45.2% < 2 years) and became significantly less important over time (11% of > 20 years, p < 0.001). Most commonly cited movement symptoms were difficulties with walking and balance (44%) which peaked in the 11–20 year group (60.5%, p < 0.001), and slow movements (30.6%) which stayed generally constant.
PwP1: Getting around is my biggest problem and it impacts my whole life, from getting around the house to getting out and about and socializing.
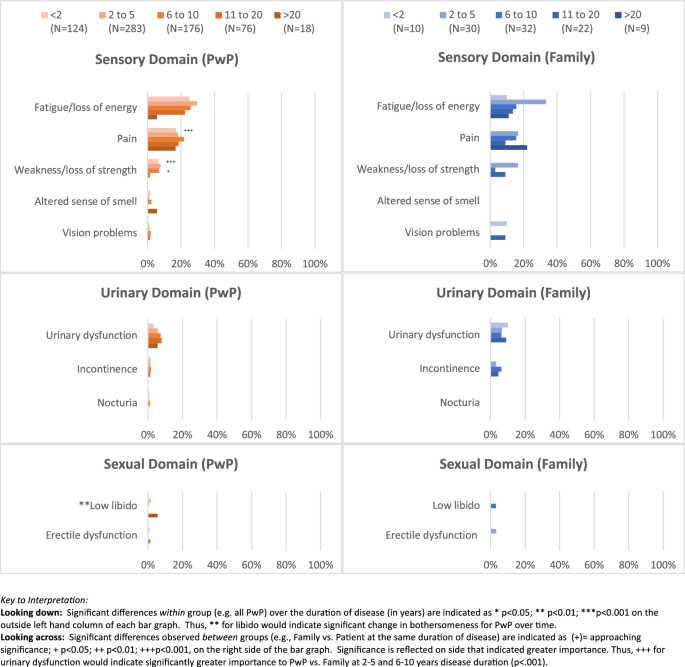
Nearly 50% of PwP reported concurrent functional mobility impacts, with the most affected areas being ability to exercise and engage in sports (27.1% overall) such as cycling, yoga, hiking, followed by threats to safety (13.1%; tripping and falling or hurting oneself accidentally). Other issues of mobility outside of walking (e.g., turning in bed, getting up from sitting, standing, stairs) were infrequently cited as bothersome (< 2.4%).
PwP2: I miss being able to go for a walk without a walker and being afraid of falling.
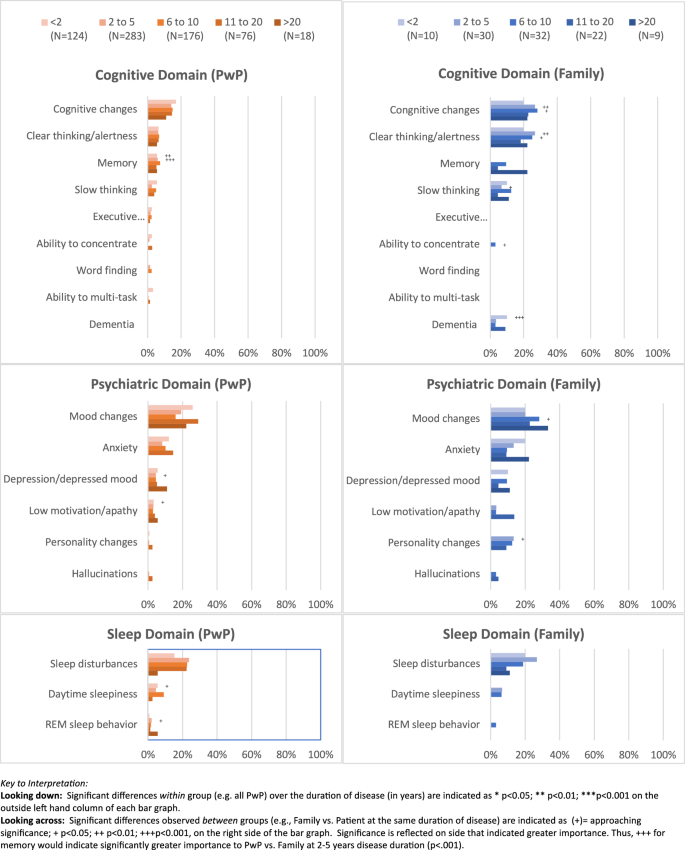
At all stages, the most bothersome symptoms included fatigue (26.7%), mood changes (20.8%), pain (18.4%), changes to thinking (14.7%) and speech difficulties (13.1%). These affected relationships with others (27.4%) pleasurable activities (23.2%), social life (22.9%) ability to communicate (12.7%) and ability to perform responsibilities and obligations (e.g., job functions; 9.3%). The frequency of reported bothersomeness generally increased over time in these areas.
PwP3: By the time I have formed words, others have moved on and I often do not get a chance to speak.
Sleep related problems were also important to many (21.2%) and were reported more often at later PD stages. A substantial proportion of PwP cited general mood changes as highly bothersome (20.8%)—most commonly anxiety (9.9%) versus depression (5.2%) or apathy (3.1%).
PwP4: Constantly having to fight fatigue and stiffness affects the ability to rest and relax and constantly trying to achieve anything is depressing.
PwP5: Sleeping is a thing of the past and makes me unable to fight the battle the next day. It depletes my energy and strength.
Cumulatively, these experiences contributed to an overall increased work of living (45.5%) with participants reporting it took longer to do things and required greater intentionality for activities that were previously intuitive and automatic. Personal coping (38.4%) and personal self-concept (31.5%) were often negatively affected with sense of greater dependence on others (15.7%).
PwP6: These affect almost everything I do—makes life seem a bit of a struggle.
PwP7: The length of time it takes to do ordinary tasks such as showering and getting dressed are a constant problem. Getting up and getting dressed used to take a matter of 5 to 10 min in the good old days before I had PD, but now [it’s] an hour. Buttoning my shirt or tying my shoelaces … can leave me feeling tired before my day has even begun.
PwP8: These prevent me doing what I enjoy—walking my dog, gardening, driving, throwing parties for friends and more!
PwP9: Loss of independence is humiliating and loss of [my] self-worth.
PwP10: I cannot make it different no matter how much effort I make! It is so frustrating!!!!!
Contextual factors were also important to the PD experience, most commonly frequency and severity of symptoms (66%). Nearly 48% of participants explicitly stated that their most important experiences were those that had the biggest functional impact and were their most common symptom (29.9%). A deep desire for improved PD management (e.g., better medications, diagnosis) was listed by 20.8% of respondents as important aspects of the PD experience:
PwP11: The medication to treat Parkinson’s is not effective.
PwP12: [We] need hope for the future and there is no hope.
Most important aspects of PD reported by family
As shown in Fig. 2a–d, top symptom concerns noted by PwP were generally shared by family. However, compared to PwP, family more often prioritized functional impact of PD over specific symptoms. Greatest concerns centered around impact on mobility and consequences of mobility limitations. For example, while PwP were concerned for safety, family members expressed substantially more concerns that increased over time, from 20% in early PD to 50% at 11 + years (p = 0.06). Biggest differences between PwP and family member concerns for safety were observed after 11–20 years (p = 0.04). Common safety concerns included altered gait (17.4%), slow movements (13%), and freezing (10.4%) leading to falls or injury.
F83: [I’m] not happy to let him go out on his own. I’m afraid of him falling.
F18: Even simple tasks like shopping become hazardous.
F110: Her balance is bad because her limbs freeze, and this means she gets stuck on the spot without warning whilst trying to walk.
F119: My husband can’t be left in case of falls which means I’m with him 24/7.
Similar concerns were observed for diminished self-reliance and independence (20% overall) which was of greatest concern in the < 2 years group (50%) and was less frequently cited with longer disease duration. Concern by family members regarding PwP independence was greater than PwP in earlier disease (0–2 years; p < 0.03).
Psychosocial impacts were also more commonly reported by family (80.9%) than PwP (65.7%). These included cognitive, mood, and personality changes, with functional impacts on self-concept, social life, and quality of life, among others (eTable 2).
F106: The crippling anxiety has taken a terrible toll on all aspects of our lives…He has been suicidal, avoids family and friends, he is totally self-absorbed… and it’s heartbreaking to watch and not be able to help.
Worry about cognitive symptoms were reported by family at all stages and increased after the first two years. Important cognitive changes included decline in mental alertness (23.5%), slow thinking (7.8%), and memory loss (7.8%). Other significant differences included concerns about personality changes, which was most notably different in the 2–5 years range (p < 0.05). Family members cited general mood changes (26.1%) low motivation or apathy (17.4%), and anxiety (13%) at a much higher rate than PwP, as seen here:
F87: My husband has the rigid type of PD, but I notice more the cognitive issues and slowness of thought. He notices this less which is a blessing!
F77: Most difficult aspect for us are the psychological aspects, in particular attacks of anxiety/panic. Mood swings can be very sudden and difficult to deal with.
For all stages, family members reported that PD substantially impacted interpersonal interactions (60%). This included specific impacts on social life (28.7%), communication (27%), ability to engage in pleasurable activities (27.8%), and relationships with others (18.3%). Interpersonal challenges were reported significantly more often at nearly all stages of disease by family compared to PwP.
F85: I cannot hold a conversation with him as he forgets the words he was going to say.
F17: Losing his speech was devastating for him… which made him feel worthless.
F88: The[se] symptoms have the most negative affect on our everyday lives, our ability to do anything, and detrimentally affect our relationship.
Similarly, many family members (29%) indicated concerns about impact on self-concept, indicating that PD symptoms contributed to feelings of embarrassment or being stigmatized while in public and sometimes resulted in social isolation (14.8% overall). Isolation was most often reported by family during early PD years (30%, p < 0.001) with diminished reporting over time. In contrast PwP generally reported experiencing isolation later in disease (> 10 years duration).
F37: These have a big effect on our lives – not wanting to go places; giving up activities due to lack of self-confidence; increasingly not wanting to go places by oneself, even to familiar places.
F83: Outside people don’t always have the patience to wait and give him time to move and say what he wants to.
Overall, concerns for impact on PwP quality of life (QoL) were generally similar between family and PwP (30% vs. 36%, respectively). Greatest differences were found between the PwP perception of the extent to which PD impacted their partner’s QoL vs. family’s perception. More than 36% of all family members expressed substantial personal difficulty coping with the decline in physical and psychosocial functioning of the PwP, which was most notable in earlier (50% < 2 years) and later disease (56% > 20 years) and was significantly greater than PwP perceptions at all stages of disease.
F122: I am constantly exhausted.
F58: I feel like I’m losing her [mum] day by day.
Discussion
This is the first large-scale international survey to explore perceptions of important aspects of PD in people with PD versus family members and how these may change with longer duration of disease. Prior knowledge in this area has been mostly derived from smaller qualitative interview studies that have focused on prevalence rather than importance of symptoms3,15,16,17. To date, only one other large study (Fox Insight PD-PROP) has gathered large scale qualitative survey evidence of most bothersome symptoms18. However this study did not compare perspectives of families and caregivers, as in the present study. Previous evidence along with findings from the current study suggests that prevalence is not synonymous with importance, and that some symptoms may be often present but less frequently meaningful15. For example, high prevalence has been observed for drooling and altered sense of smell19, which has been reported as being comparatively less important to PwP than other symptoms that cause specific functional impairments3,15. Thus, selection of relevant concepts for clinical trials should consider prevalence alongside relative importance.
In this study, several notable differences were observed between PwP and family perceptions of what mattered. In general, family members were less likely to focus on individual symptoms than PwP and tended to prioritize changes in thinking and functioning that PwP were less observant of, particularly in later stages, which is consistent with prior reports20. Conversely, PwP at all stages reported greater concerns for symptoms that were less apparent to family, such as pain, fatigue, and work of living (i.e., the effort needed to complete daily living activities)21. Existence of perceptual differences have been reported in prior work22, and point to a need for holistic evaluation of PD symptoms and impacts, combining observer and personal report, even at earliest stages of disease.
In this study, we observed that movement-related symptoms, which affected both physical and psychosocial functioning from earliest PD onwards, were consistently cited as important and did not appear to change significantly as a function of age. As expected, walking and balance, freezing of gait, and dyskinesias generally did become more important with longer PD duration, along with concerns for functional mobility23. In contrast, tremor became substantially less important over time4, while perceptions of fine motor and slow movement remained stable and were equally important from onset throughout the course of PD. As data from this study focused solely on what was important, it is not clear whether the severity of symptoms also changed, or how normalization of chronic symptoms and other contextual factors (e.g., retirement) might contribute to changing perceptions over time.
Consistent with prior research, other most important non motor symptoms included mood, sleep, cognitive, and speech changes24,25. Greatest concerns were noted with speech and communication over time, whereas concern with cognition and mood changes tended to remain stable. Personality changes were also common with later disease and generally more observable to family than PwP. Pain and fatigue were bothersome at all stages, while sleep appeared less bothersome in later PD than early on. The frequent reporting of these symptoms and related impacts highlights the importance of non-motor experiences for people with PD at all stages and aligns with growing recognition of PD as multi-system disorder26,27.
Lastly, although not specifically designed to explore family burden, we observed substantial impact in this area that was evident from family responses. Our data suggest that family burden and diminished quality of life—both individually and as a couple—may be due to increased interpersonal and relationship difficulties, altered communication, and diminished ability to engage in pleasurable activities such as traveling, dining out or hobbies. Caregiver burden has been recognized as an issue in later disease PD28,29,30, however, our findings suggest a high level of burden at early stages, some of which appears anticipatory31. Thus, greater attention to formalized family support from early disease onwards may be warranted8,10,32, which has been suggested for other chronic, progressive illnesses as well33,34.
Limitations of this study include self-identification of PD, which may be different from the actual diagnosis and onset of PD, a predominantly white population with limited demographic information to characterize findings, and low total response rates similar to other online surveys35; therefore, findings should be interpreted with caution. In particular, the use of a non-dyadic data collection approaches (unrelated PwP and family respondents) limits ability to assess the extent to which individuals from the same family unit align or differ perceptually. This information is greatly needed to understand the reliability of patient self-reporting as prior studies have identified discrepancies in symptom perceptions in patients with greater cognitive impairment36. Furthermore, individuals with later-stage PD might have reduced ability to participate in survey-based research. Future research using dyadic approaches to data collection and more in-depth participant characterization will be needed to better understand differences in perceptions and how this might change with time and disease progression. Assessing patients along with key informants longitudinally can help to evaluate accuracy of self-reporting vs care-partner feedback at different stages of disease and has been successful in other cognitive disorders such as Alzheimer’s disease37,38,39. Similar approaches would be informative for PD, particularly if correlated with biomarkers of disease progression40. Despite the noted limitations, we believe the findings presented here are useful in understanding what matters to people affected by Parkinson’s, how this may change over time, and alignment between PwP and family members.
Conclusion
Important differences may exist regarding what matters to PwP vs. family members and appear to change with longer duration of disease. Understanding important versus prevalent symptoms and functional impacts can support clinical care relevant to different stages of PD, research focused on development of outcomes measures that reflect what matters most to people affected by PD, and clinical trials of promising new therapies targeting underlying biology. Inclusion of family perspectives from earliest stages may aid in broader understanding of functional impacts and development of interventions to preserve capacity.
Data availability
Full data with qualitative content coding are available as supplemental materials.
References
-
USDHHS, Patient-focused drug development: Selecting, Developing, or Modifying Fit-for-Purpose Clinical Outcome Assessments (Guidance 3), https://www.fda.gov/regulatory-information/search-fda-guidance-documents/patient-focused-drug-development-selecting-developing-or-modifying-fit-purpose-clinical-outcome. (2022).
-
Mammen, J. et al. Mapping meaningful symptoms and impacts of disease to digital outcome measures. J. Parkinsons Dis. 13(4), 589–607. https://doi.org/10.3233/JPD-225122 (2023).
-
Politis, M. et al. Parkinson’s disease symptoms: The patient’s perspective. Mov. Disord. 25, 1646–1651 (2010).
-
Port, R. J. et al. People with Parkinson’s disease: What symptoms do they most want to improve and how does this change with disease duration?. J. Parkinsons Dis. 11, 715–724 (2021).
-
USDHHS, Patient-focused drug development: Methods to identify what is important to patients (Guidance 2), https://www.fda.gov/regulatory-information/search-fda-guidance-documents/patient-focused-drug-development-methods-identify-what-important-patients. (2022).
-
Chalasani, M., Vaidya, P. & Mullin, T. Enhancing the incorporation of the patient’s voice in drug development and evaluation. Res. Involv. Engagem. 4, 10 (2018).
-
McFarthing, K. et al. Parkinson’s disease drug therapies in the clinical trial pipeline: 2023 update. J. Parkinsons Dis. 13, 427–439 (2023).
-
Geerlings, A. D. et al. Caregiver burden in Parkinson’s disease: A mixed-methods study. BMC Med. 21, 247 (2023).
-
Lubomski, M., Davis, R. L. & Sue, C. M. Health-related quality of life for Parkinson’s disease patients and their caregivers. J. Mov. Disord. 14, 42–52 (2021).
-
Theed, R., Eccles, F. & Simpson, J. Experiences of caring for a family member with Parkinson’s disease: A meta-synthesis. Aging Ment. Health 21, 1007–1016 (2017).
-
(2013) World Medical Association Declaration of Helsinki ethical principles for medical research involving human subjects. JAMA J. Am. Med. Assoc. 310, 2191–2194.
-
Mammen, J. et al. A consensus conceptual model of early Parkinson’s disease. Res. Square. https://doi.org/10.21203/rs.3.rs-4377805/v1 (2024).
-
Akoglu, H. User’s guide to correlation coefficients. Turk. J. Emerg. Med. 18, 91–93 (2018).
-
O’Brien, B. C., Harris, I. B., Beckman, T. J., Reed, D. A. & Cook, D. A. Standards for reporting qualitative research: A synthesis of recommendations. Acad. Med. 89, 1245–1251 (2014).
-
Mammen, J. et al. Relative meaningfulness and impacts of symptoms in people with early-stage Parkinson’s disease. J. Parkinsons Disease 13, 619–632 (2023).
-
Morel, T. et al. Patient experience in early-stage Parkinson’s disease: Using a mixed methods analysis to identify which concepts are cardinal for clinical trial outcome assessment. Neurol. Ther. 11, 1319–1340 (2022).
-
Staunton, H. et al. A patient-centered conceptual model of symptoms and their impact in early Parkinson’s disease: A qualitative study. J. Parkinsons Disease 12, 137–151 (2022).
-
Marras, C. et al. What patients say: Large-scale analyses of replies to the Parkinson’s disease patient report of problems (PD-PROP). J. Parkinsons Dis. 13, 757–767 (2023).
-
Muller, B. et al. Autonomic symptoms and dopaminergic treatment in de novo Parkinson’s disease. Acta Neurologica Scandinavica 127, 290–294 (2013).
-
Siciliano, M. et al. Correlates of the discrepancy between objective and subjective cognitive functioning in non-demented patients with Parkinson’s disease. J. Neurol. 268, 3444–3455 (2021).
-
Naisby, J. et al. A survey of people with Parkinson’s and their carers: The management of pain in Parkinson’s. J. Geriatr. Psychiatry Neurol. 35, 613–621 (2022).
-
Tosin, M. H., Goetz, C. G. & Stebbins, G. T. Patient with Parkinson disease and care partner perceptions of key domains affecting health-related quality of life: Systematic review. Neurology 102, e208028 (2024).
-
Wilson, J. et al. Gait progression over 6 years in Parkinson’s disease: Effects of age, medication, and pathology. Front. Aging Neurosci. 12, 577435 (2020).
-
Pan, C. X. et al. Subjective cognitive complaints in newly-diagnosed Parkinson’s disease with and without mild cognitive impairment. Front. Neurosci. 15, 8 (2021).
-
Koh, M. R. E. et al. Poor sleep quality is associated with fatigue and depression in early Parkinson’s disease: A longitudinal study in the PALS cohort. Front. Neurol. 13, 9 (2022).
-
Costa, H. N., Esteves, A. R., Empadinhas, N. & Cardoso, S. M. Parkinson’s disease: A multisystem disorder. Neurosci. Bull. 39, 113–124 (2023).
-
Muller, B., Assmus, J., Herlofson, K., Larsen, J. P. & Tysnes, O. B. Importance of motor vs. non-motor symptoms for health-related quality of life in early Parkinson’s disease. Parkinsonism Related Disord. 19, 1027–1032 (2013).
-
Macchi, Z. A. et al. Patient and caregiver characteristics associated with caregiver burden in Parkinson’s disease: A palliative care approach. Ann. Palliat. Med. 9, S24–S33 (2020).
-
Rosqvist, K., Schrag, A., Odin, P. & The CLaSP Consortium. Caregiver burden and quality of life in late stage Parkinson’s disease. Brain Sci. 12(1), 111. https://doi.org/10.3390/brainsci12010111 (2022).
-
Tan, Q. Y. et al. The experiences of treatment burden in people with Parkinson’s disease and their caregivers: A systematic review of qualitative studies. J. Parkinsons Dis. 11, 1597–1617 (2021).
-
Fox, S., Azman, A. & Timmons, S. Palliative care needs in Parkinson’s disease: Focus on anticipatory grief in family carers. Ann. Palliat. Med. 9, S34–S43 (2020).
-
Navarta-Sanchez, M. V. et al. Perspectives of people with Parkinson’s disease and family carers about disease management in community settings: A cross-country qualitative study. J. Clin. Nurs. 32, 5201–5218 (2023).
-
Jika, B. M., Khan, H. T. A. & Lawal, M. Exploring experiences of family caregivers for older adults with chronic illness: A scoping review. Geriatr. Nurs. 42, 1525–1532 (2021).
-
Sautter, J. M. et al. Caregiver experience during advanced chronic illness and last year of life. J. Am. Geriatr. Soc. 62, 1082–1090 (2014).
-
Wu, M.-J., Zhao, K. & Fils-Aime, F. Response rates of online surveys in published research: A meta-analysis. Comput. Hum. Behav. Rep. 7, 100206 (2022).
-
Sands, L. P., Ferreira, P., Stewart, A. L., Brod, M. & Yaffe, K. What Explains differences between dementia patients’ and their caregivers’ ratings of patients’ quality of life?. Am. J. Geriatr. Psychiatry 12, 272–280 (2004).
-
Nosheny, R. L. et al. The role of dyadic cognitive report and subjective cognitive decline in early ADRD clinical research and trials: Current knowledge, gaps, and recommendations. Alzheimers Dement (N Y) 8, e12357 (2022).
-
Nuno, M. M., Gillen, D. L., Grill, J. D. & Alzheimer’s Disease Cooperative, S. Study partner types and prediction of cognitive performance: Implications to preclinical Alzheimer’s trials. Alzheimers Res. Ther. 11, 92 (2019).
-
Wadley, V. G., Harrell, L. E. & Marson, D. C. Self- and informant report of financial abilities in patients with Alzheimer’s disease: Reliable and valid?. J. Am. Geriatr. Soc. 51, 1621–1626 (2003).
-
Simuni, T. et al. A biological definition of neuronal alpha-synuclein disease: Towards an integrated staging system for research. Lancet Neurol. 23, 178–190 (2024).
Acknowledgements
This study was sponsored by the Michael J Fox Foundation for Parkinson’s Research (Grant # MJFF-024452). The authors would like to thank MJFF as sponsor and Parkinson’s UK for sharing data. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement by the Critical Path, US FDA, MJFF, Parkinson’s UK or any other agency.
Author information
Authors and Affiliations
Contributions
Data analysis was conducted by JRM and MT. Interpretation, writing, and revising the manuscript were performed by all authors (JRM, MT, JC, JLA, YX, DS, CB).
Corresponding author
Ethics declarations
Competing interests
All authors declare no financial or non-financial competing interests for the study. JRM has consulted for and received research funding from the Michael J Fox Foundation for Parkinson’s Research. JLA Has received honoraria from Huntington Study Group, research support from National Institutes of Health, The Michael J Fox Foundation for Parkinson’s Research, Biogen, Safra Foundation, Empire Clinical Research Investigator Program, and consultancy fees from VisualDx.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mammen, J.R., Tyo, M., Cadorette, J. et al. Understanding what aspects of Parkinson’s disease matter most to patients and families. Sci Rep 14, 21171 (2024). https://doi.org/10.1038/s41598-024-71555-4
-
Received:
-
Accepted:
-
Published:
-
DOI: https://doi.org/10.1038/s41598-024-71555-4
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.