Cook A, Bono F, Jinek M, Conti E. Structural biology of nucleocytoplasmic transport. Annu Rev Biochem. 2007;76:647–71.
Doye V, Hurt E. From nucleoporins to nuclear pore complexes. Curr Opin Cell Biol. 1997;9(3):401–11.
Ptak C, Aitchison JD, Wozniak RW. The multifunctional nuclear pore complex: a platform for controlling gene expression. Curr Opin Cell Biol. 2014;28:46–53.
Ribbeck K, Görlich D. The permeability barrier of nuclear pore complexes appears to operate via hydrophobic exclusion. EMBO J. 2002;21(11):2664–71.
Toyama B, Arrojo e Drigo R, Lev-Ram V, Ramachandra R, Deerinck T, Lechene C, Ellisman M, Hetzer M. Visualization of long-lived proteins reveals age mosaicism within nuclei of postmitotic cells. J Cell Biol. 2018;218:jcb201809123.
Hetzer MW. The role of the nuclear pore complex in aging of post-mitotic cells. Aging. 2010;2(2):74–5.
Savas JN, Toyama BH, Xu T, Yates JR 3rd, Hetzer MW. Extremely long-lived nuclear pore proteins in the rat brain. Science. 2012;335(6071):942.
Spead O, Zaepfel BL, Rothstein JD. Nuclear Pore Dysfunction in Neurodegeneration. Neurotherapeutics. 2022;19(4):1050–60.
Cristi AC, Rapuri S, Coyne AN. Nuclear pore complex and nucleocytoplasmic transport disruption in neurodegeneration. FEBS Lett. 2023.
Patel V, Chu C. Nuclear transport, oxidative stress, and neurodegeneration. Int J Clin Exp Pathol. 2011;4:215–29.
Devos D, Dokudovskaya S, Williams R, Alber F, Eswar N, Chait BT, Rout MP, Sali A. Simple Fold composition and modular architecture of the nuclear pore complex. Proc Natl Acad Sci U S A. 2006;103(7):2172–7.
Lin DH, Hoelz A. The structure of the Nuclear Pore Complex (an update). Annu Rev Biochem. 2019;88:725–83.
von Appen A, Beck M. Structure determination of the Nuclear Pore Complex with three-dimensional Cryo electron Microscopy. J Mol Biol. 2016;428(10 Pt A):2001–10.
Hakhverdyan Z, Molloy KR, Keegan S, Herricks T, Lepore DM, Munson M, Subbotin RI, Fenyö D, Aitchison JD, Fernandez-Martinez J, et al. Dissecting the Structural dynamics of the Nuclear Pore Complex. Mol Cell. 2021;81(1):153–e165157.
Denning DP, Patel SS, Uversky V, Fink AL, Rexach M. Disorder in the nuclear pore complex: the FG repeat regions of nucleoporins are natively unfolded. Proc Natl Acad Sci U S A. 2003;100(5):2450–5.
Strawn LA, Shen T, Shulga N, Goldfarb DS, Wente SR. Minimal nuclear pore complexes define FG repeat domains essential for transport. Nat Cell Biol. 2004;6(3):197–206.
Dekker M, Van der Giessen E, Onck PR. Phase separation of intrinsically disordered FG-Nups is driven by highly dynamic FG motifs. Proceedings of the National Academy of Sciences. 2023, 120(25):e2221804120.
Khalil B, Linsenmeier M, Smith CL, Shorter J, Rossoll W. Nuclear-import receptors as gatekeepers of pathological phase transitions in ALS/FTD. Mol Neurodegener. 2024;19(1):8.
Beck M, Hurt E. The nuclear pore complex: understanding its function through structural insight. Nat Rev Mol Cell Biol. 2017;18(2):73–89.
Bui Khanh H, von Appen A, DiGuilio Amanda L, Ori A, Sparks L, Mackmull M-T, Bock T, Hagen W, Andrés-Pons A, Glavy Joseph S, et al. Integrated Structural Analysis of the Human Nuclear Pore Complex Scaffold. Cell. 2013;155(6):1233–43.
Kampmann M, Blobel G. Three-dimensional structure and flexibility of a membrane-coating module of the nuclear pore complex. Nat Struct Mol Biol. 2009;16(7):782–8.
Boehmer T, Enninga J, Dales S, Blobel G, Zhong H. Depletion of a single nucleoporin, Nup107, prevents the assembly of a subset of nucleoporins into the nuclear pore complex. Proc Natl Acad Sci. 2003;100(3):981–5.
Walther TC, Alves A, Pickersgill H, Loïodice I, Hetzer M, Galy V, Hülsmann BB, Köcher T, Wilm M, Allen T, et al. The conserved Nup107-160 complex is critical for nuclear pore complex assembly. Cell. 2003;113(2):195–206.
Fernandez-Martinez J, Rout MP. One Ring to rule them all? Structural and functional diversity in the Nuclear Pore Complex. Trends Biochem Sci. 2021;46(7):595–607.
Eisenhardt N, Redolfi J, Antonin W. Interaction of Nup53 with Ndc1 and Nup155 is required for nuclear pore complex assembly. J Cell Sci. 2014;127(Pt 4):908–21.
Mosalaganti S, Obarska-Kosinska A, Siggel M, Taniguchi R, Turoňová B, Zimmerli CE, Buczak K, Schmidt FH, Margiotta E, Mackmull M-T, et al. AI-based structure prediction empowers integrative structural analysis of human nuclear pores. Science. 2022;376(6598):eabm9506.
Sakuma S, Raices M, Borlido J, Guglielmi V, Zhu EYS, D’Angelo MA. Inhibition of nuclear pore complex formation selectively induces Cancer Cell Death. Cancer Discov. 2021;11(1):176–93.
Funakoshi T, Maeshima K, Yahata K, Sugano S, Imamoto F, Imamoto N. Two distinct human POM121 genes: requirement for the formation of nuclear pore complexes. FEBS Lett. 2007;581(25):4910–6.
Bindra D, Mishra RK. In pursuit of distinctiveness: transmembrane nucleoporins and their Disease associations. Front Oncol. 2021;11:784319.
Mansfeld J, Güttinger S, Hawryluk-Gara LA, Panté N, Mall M, Galy V, Haselmann U, Mühlhäusser P, Wozniak RW, Mattaj IW, et al. The conserved transmembrane nucleoporin NDC1 is required for nuclear pore complex assembly in vertebrate cells. Mol Cell. 2006;22(1):93–103.
Kind B, Koehler K, Lorenz M, Huebner A. The nuclear pore complex protein ALADIN is anchored via NDC1 but not via POM121 and GP210 in the nuclear envelope. Biochem Biophys Res Commun. 2009;390(2):205–10.
Funakoshi T, Clever M, Watanabe A, Imamoto N. Localization of Pom121 to the inner nuclear membrane is required for an early step of interphase nuclear pore complex assembly. Mol Biol Cell. 2011;22(7):1058–69.
Talamas JA, Hetzer MW. POM121 and Sun1 play a role in early steps of interphase NPC assembly. J Cell Biol. 2011;194(1):27–37.
Mitchell JM, Mansfeld J, Capitanio J, Kutay U, Wozniak RW. Pom121 links two essential subcomplexes of the nuclear pore complex core to the membrane. J Cell Biol. 2010;191(3):505–21.
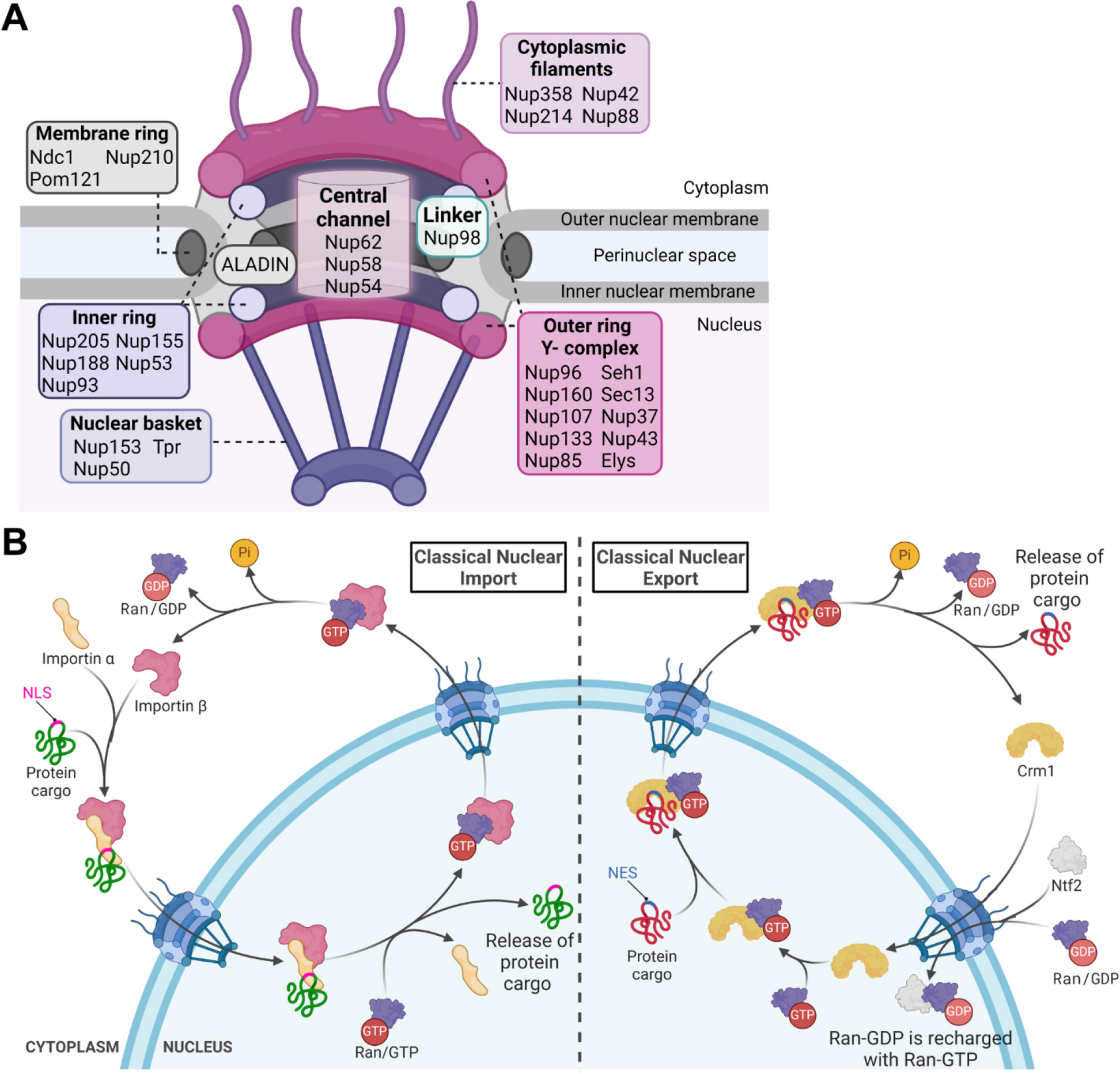
Hu T, Guan T, Gerace L. Molecular and functional characterization of the p62 complex, an assembly of nuclear pore complex glycoproteins. J Cell Biol. 1996;134(3):589–601.
Chug H, Trakhanov S, Hülsmann BB, Pleiner T, Görlich D. Crystal structure of the metazoan Nup62•Nup58•Nup54 nucleoporin complex. Science. 2015;350(6256):106–10.
Hampoelz B, Andres-Pons A, Kastritis P, Beck M. Structure and assembly of the Nuclear Pore Complex. Annual Rev Biophys. 2019;48(1):515–36.
Finlay DR, Meier E, Bradley P, Horecka J, Forbes DJ. A complex of nuclear pore proteins required for pore function. J Cell Biol. 1991;114(1):169–83.
Percipalle P, Clarkson WD, Kent HM, Rhodes D, Stewart M. Molecular interactions between the importin α/β heterodimer and proteins involved in vertebrate nuclear protein import11Edited by J. Karn. J Mol Biol. 1997;266(4):722–32.
Macara IG. Transport into and out of the nucleus. Microbiol Mol Biol Rev. 2001;65(4):570–94. table of contents.
Terry LJ, Wente SR. Flexible gates: dynamic topologies and functions for FG nucleoporins in nucleocytoplasmic transport. Eukaryot Cell. 2009;8(12):1814–27.
Solmaz SR, Chauhan R, Blobel G, Melčák I. Molecular architecture of the transport channel of the nuclear pore complex. Cell. 2011;147(3):590–602.
Kabachinski G, Schwartz TU. The nuclear pore complex–structure and function at a glance. J Cell Sci. 2015;128(3):423–9.
Frey S, Richter RP, Görlich D. FG-Rich repeats of Nuclear Pore proteins Form a three-Dimensional Meshwork with Hydrogel-Like Properties. Science. 2006;314(5800):815–7.
Hülsmann Bastian B, Labokha Aksana A, Görlich D. The permeability of Reconstituted Nuclear pores provides direct evidence for the selective phase model. Cell. 2012;150(4):738–51.
Ng SC, Biswas A, Huyton T, Schünemann J, Reber S, Görlich D. Barrier properties of Nup98 FG phases ruled by FG motif identity and inter-FG spacer length. Nat Commun. 2023;14(1):747.
Petrovic S, Samanta D, Perriches T, Bley CJ, Thierbach K, Brown B, Nie S, Mobbs GW, Stevens TA, Liu X, et al. Architecture of the linker-scaffold in the nuclear pore. Science. 2022;376(6598):eabm9798.
Oka M, Asally M, Yasuda Y, Ogawa Y, Tachibana T, Yoneda Y. The mobile FG nucleoporin Nup98 is a cofactor for Crm1-dependent protein export. Mol Biol Cell. 2010;21(11):1885–96.
Bangs P, Burke B, Powers C, Craig R, Purohit A, Doxsey S. Functional analysis of Tpr: identification of nuclear pore complex association and nuclear localization domains and a role in mRNA export. J Cell Biol. 1998;143(7):1801–12.
Guan T, Kehlenbach RH, Schirmer EC, Kehlenbach A, Fan F, Clurman BE, Arnheim N, Gerace L. Nup50, a nucleoplasmically oriented nucleoporin with a role in nuclear protein export. Mol Cell Biol. 2000;20(15):5619–30.
Panté N, Aebi U. Molecular dissection of the Nuclear Pore Complex. Crit Rev Biochem Mol Biol. 1996;31(2):153–99.
Hoelz A, Debler EW, Blobel G. The structure of the nuclear pore complex. Annu Rev Biochem. 2011;80:613–43.
Krull S, Thyberg J, Björkroth B, Rackwitz HR, Cordes VC. Nucleoporins as components of the nuclear pore complex core structure and tpr as the architectural element of the nuclear basket. Mol Biol Cell. 2004;15(9):4261–77.
Tingey M, Li Y, Yu W, Young A, Yang W. Spelling out the roles of individual nucleoporins in nuclear export of mRNA. Nucleus (Calcutta). 2022;13(1):172–95.
David-Watine B. Silencing nuclear pore protein Tpr elicits a senescent-like phenotype in cancer cells. PLoS ONE. 2011;6(7):e22423.
Zhao CL, Mahboobi SH, Moussavi-Baygi R, Mofrad MR. The interaction of CRM1 and the nuclear pore protein Tpr. PLoS ONE. 2014;9(4):e93709.
McCloskey A, Ibarra A, Hetzer MW. Tpr regulates the total number of nuclear pore complexes per cell nucleus. Genes Dev. 2018;32(19–20):1321–31.
Lindsay ME, Plafker K, Smith AE, Clurman BE, Macara IG. Npap60/Nup50 is a tri-stable switch that stimulates importin-alpha:beta-mediated nuclear protein import. Cell. 2002;110(3):349–60.
Makise M, Mackay DR, Elgort S, Shankaran SS, Adam SA, Ullman KS. The Nup153-Nup50 protein interface and its role in nuclear import. J Biol Chem. 2012;287(46):38515–22.
Duheron V, Chatel G, Sauder U, Oliveri V, Fahrenkrog B. Structural characterization of altered nucleoporin Nup153 expression in human cells by thin-section electron microscopy. Nucleus (Calcutta). 2014;5(6):601–12.
Li P, Noegel AA. Inner nuclear envelope protein SUN1 plays a prominent role in mammalian mRNA export. Nucleic Acids Res. 2015;43(20):9874–88.
Walther TC, Fornerod M, Pickersgill H, Goldberg M, Allen TD, Mattaj IW. The nucleoporin Nup153 is required for nuclear pore basket formation, nuclear pore complex anchoring and import of a subset of nuclear proteins. EMBO J. 2001;20(20):5703–14.
Lenz-Böhme B, Wismar J, Fuchs S, Reifegerste R, Buchner E, Betz H, Schmitt B. Insertional mutation of the Drosophila nuclear lamin Dm0 gene results in defective nuclear envelopes, clustering of nuclear pore complexes, and accumulation of annulate lamellae. J Cell Biol. 1997;137(5):1001–16.
Bley CJ, Nie S, Mobbs GW, Petrovic S, Gres AT, Liu X, Mukherjee S, Harvey S, Huber FM, Lin DH, et al. Architecture of the cytoplasmic face of the nuclear pore. Science. 2022;376(6598):eabm9129.
Werner A, Flotho A, Melchior F. The RanBP2/RanGAP1∗SUMO1/Ubc9 complex is a multisubunit SUMO E3 ligase. Mol Cell. 2012;46(3):287–98.
Mahadevan K, Zhang H, Akef A, Cui XA, Gueroussov S, Cenik C, Roth FP, Palazzo AF. RanBP2/Nup358 potentiates the translation of a subset of mRNAs encoding secretory proteins. PLoS Biol. 2013;11(4):e1001545.
Fornerod M, van Deursen J, van Baal S, Reynolds A, Davis D, Murti KG, Fransen J, Grosveld G. The human homologue of yeast CRM1 is in a dynamic subcomplex with CAN/Nup214 and a novel nuclear pore component Nup88. EMBO J. 1997;16(4):807–16.
Katahira J, Strässer K, Podtelejnikov A, Mann M, Jung JU, Hurt E. The Mex67p-mediated nuclear mRNA export pathway is conserved from yeast to human. EMBO J. 1999;18(9):2593–609.
Kendirgi F, Rexer DJ, Alcázar-Román AR, Onishko HM, Wente SR. Interaction between the shuttling mRNA export factor Gle1 and the nucleoporin hCG1: a conserved mechanism in the export of Hsp70 mRNA. Mol Biol Cell. 2005;16(9):4304–15.
von Moeller H, Basquin C, Conti E. The mRNA export protein DBP5 binds RNA and the cytoplasmic nucleoporin NUP214 in a mutually exclusive manner. Nat Struct Mol Biol. 2009;16(3):247–54.
Alcázar-Román AR, Tran EJ, Guo S, Wente SR. Inositol hexakisphosphate and Gle1 activate the DEAD-box protein Dbp5 for nuclear mRNA export. Nat Cell Biol. 2006;8(7):711–6.
Ren Y, Seo H-S, Blobel G, Hoelz A. Structural and functional analysis of the interaction between the nucleoporin Nup98 and the mRNA export factor Rae1. Proc Nat Acad Sci. 2010, 107(23):10406–10411.
Rajoo S, Vallotton P, Onischenko E, Weis K. Stoichiometry and compositional plasticity of the yeast nuclear pore complex revealed by quantitative fluorescence microscopy. Proc Natl Acad Sci. 2018;115(17):E3969–77.
Kim SJ, Fernandez-Martinez J, Nudelman I, Shi Y, Zhang W, Raveh B, Herricks T, Slaughter BD, Hogan JA, Upla P, et al. Integrative structure and functional anatomy of a nuclear pore complex. Nature. 2018;555(7697):475–82.
Nuclear Pore Complexes: Global Conservation and Local Variation. Curr Biol. 2018, 28(11):R674-R677.
Tran EJ, Wente SR. Dynamic nuclear pore complexes: life on the Edge. Cell. 2006;125(6):1041–53.
Beck M, Förster F, Ecke M, Plitzko JM, Melchior F, Gerisch G, Baumeister W, Medalia O. Nuclear Pore Complex structure and Dynamics revealed by Cryoelectron Tomography. Science. 2004;306(5700):1387–90.
Sakiyama Y, Mazur A, Kapinos LE, Lim RYH. Spatiotemporal dynamics of the nuclear pore complex transport barrier resolved by high-speed atomic force microscopy. Nat Nanotechnol. 2016;11(8):719–23.
D’Angelo MA, Raices M, Panowski SH, Hetzer MW. Age-dependent deterioration of nuclear pore complexes causes a loss of nuclear integrity in postmitotic cells. Cell. 2009;136(2):284–95.
Toyama Brandon H, Savas Jeffrey N, Park Sung K, Harris Michael S, Ingolia Nicholas T, Yates John R III. Hetzer Martin W: identification of long-lived proteins reveals exceptional Stability of essential Cellular structures. Cell. 2013;154(5):971–82.
Rabut G, Doye V, Ellenberg J. Mapping the dynamic organization of the nuclear pore complex inside single living cells. Nat Cell Biol. 2004;6(11):1114–21.
Timney BL, Raveh B, Mironska R, Trivedi JM, Kim SJ, Russel D, Wente SR, Sali A, Rout MP. Simple rules for passive diffusion through the nuclear pore complex. J Cell Biol. 2016;215(1):57–76.
Cole CN, Hammell CM. Nucleocytoplasmic transport: driving and directing transport. Curr Biol. 1998;8(11):R368–72.
Wing CE, Fung HYJ, Chook YM. Karyopherin-mediated nucleocytoplasmic transport. Nat Rev Mol Cell Biol. 2022;23(5):307–28.
Izaurralde E, Kutay U, von Kobbe C, Mattaj IW, Görlich D. The asymmetric distribution of the constituents of the ran system is essential for transport into and out of the nucleus. EMBO J. 1997;16(21):6535–47.
Kalita J, Kapinos LE, Lim RYH. On the asymmetric partitioning of nucleocytoplasmic transport – recent insights and open questions. J Cell Sci 2021, 134(7).
Stewart M. Molecular mechanism of the nuclear protein import cycle. Nat Rev Mol Cell Biol. 2007;8(3):195–208.
Lui K, Huang Y. RanGTPase: a Key Regulator of nucleocytoplasmic trafficking. Mol Cell Pharmacol. 2009;1(3):148–56.
Köhler A, Hurt E. Exporting RNA from the nucleus to the cytoplasm. Nat Rev Mol Cell Biol. 2007;8(10):761–73.
Carmody SR, Wente SR. mRNA nuclear export at a glance. J Cell Sci. 2009;122(Pt 12):1933–7.
Kalverda B, Pickersgill H, Shloma VV, Fornerod M. Nucleoporins directly stimulate expression of developmental and cell-cycle genes inside the nucleoplasm. Cell. 2010;140(3):360–71.
Capelson M, Liang Y, Schulte R, Mair W, Wagner U, Hetzer MW. Chromatin-bound nuclear pore components regulate gene expression in higher eukaryotes. Cell. 2010;140(3):372–83.
Menon BB, Sarma NJ, Pasula S, Deminoff SJ, Willis KA, Barbara KE, Andrews B, Santangelo GM. Reverse recruitment: the Nup84 nuclear pore subcomplex mediates Rap1/Gcr1/Gcr2 transcriptional activation. Proc Natl Acad Sci U S A. 2005;102(16):5749–54.
D’Angelo MA. Nuclear pore complexes as hubs for gene regulation. Nucleus (Calcutta). 2018;9(1):142–8.
Ibarra A, Benner C, Tyagi S, Cool J, Hetzer MW. Nucleoporin-mediated regulation of cell identity genes. Genes Dev. 2016;30(20):2253–8.
Jacinto FV, Benner C, Hetzer MW. The nucleoporin Nup153 regulates embryonic stem cell pluripotency through gene silencing. Genes Dev. 2015;29(12):1224–38.
Vaquerizas JM, Suyama R, Kind J, Miura K, Luscombe NM, Akhtar A. Nuclear pore proteins nup153 and megator define transcriptionally active regions in the Drosophila genome. PLoS Genet. 2010;6(2):e1000846.
Capelson M. You are who your friends are—nuclear pore proteins as components of chromatin-binding complexes. FEBS Lett. 2023.
Kuhn TM, Capelson M. Nuclear pore proteins in regulation of chromatin state. Cells 2019, 8(11).
Colussi C, Grassi C. Epigenetic regulation of neural stem cells: the emerging role of Nucleoporins. Stem Cells. 2021;39(12):1601–14.
Simon M-N, Dubrana K, Palancade B. On the edge: how nuclear pore complexes rule genome stability. Curr Opin Genet Dev. 2024;84:102150.
Mackay DR, Howa AC, Werner TL, Ullman KS. Nup153 and Nup50 promote recruitment of 53BP1 to DNA repair foci by antagonizing BRCA1-dependent events. J Cell Sci. 2017;130(19):3347–59.
Moudry P, Lukas C, Macurek L, Neumann B, Heriche JK, Pepperkok R, Ellenberg J, Hodny Z, Lukas J, Bartek J. Nucleoporin NUP153 guards genome integrity by promoting nuclear import of 53BP1. Cell Death Differ. 2012;19(5):798–807.
de Miranda BR, Greenamyre JT. CHAPTER 1 etiology and Pathogenesis of Parkinson’s Disease. Oxidative stress and Redox Signalling in Parkinson’s Disease. The Royal Society of Chemistry; 2017. pp. 1–26.
Kouli A, Torsney KM, Kuan W-L. Parkinson’s Disease: Etiology, Neuropathology, and Pathogenesis. 2018.
Xia Q, Liao L, Cheng D, Duong DM, Gearing M, Lah JJ, Levey AI, Peng J. Proteomic identification of novel proteins associated with Lewy bodies. Front Biosci. 2008;13:3850–6.
Postuma RB, Aarsland D, Barone P, Burn DJ, Hawkes CH, Oertel W, Ziemssen T. Identifying prodromal Parkinson’s disease: pre-motor disorders in Parkinson’s disease. Mov Disord. 2012;27(5):617–26.
Funayama M, Nishioka K, Li Y, Hattori N. Molecular genetics of Parkinson’s disease: contributions and global trends. J Hum Genet. 2023;68(3):125–30.
Ball N, Teo WP, Chandra S, Chapman J. Parkinson’s Disease and the Environment. Front Neurol. 2019;10:218.
Pouchieu C, Piel C, Carles C, Gruber A, Helmer C, Tual S, Marcotullio E, Lebailly P, Baldi I. Pesticide use in agriculture and Parkinson’s disease in the AGRICAN cohort study. Int J Epidemiol. 2018;47(1):299–310.
Narayan S, Liew Z, Bronstein JM, Ritz B. Occupational pesticide use and Parkinson’s disease in the Parkinson Environment Gene (PEG) study. Environ Int. 2017;107:266–73.
Vellingiri B, Suriyanarayanan A, Abraham KS, Venkatesan D, Iyer M, Raj N, Gopalakrishnan AV. Influence of heavy metals in Parkinson’s disease: an overview. J Neurol. 2022;269(11):5798–811.
Hindle JV. Ageing, neurodegeneration and Parkinson’s disease. Age Ageing. 2010;39(2):156–61.
Willis AW, Roberts E, Beck JC, Fiske B, Ross W, Savica R, Van Den Eeden SK, Tanner CM, Marras C, Alcalay R, et al. Incidence of Parkinson disease in North America. Npj Parkinson’s Disease. 2022;8(1):170.
Schapira AHV, Cooper JM, Dexter D, Jenner P, Clark JB, Marsden CD. MITOCHONDRIAL COMPLEX I DEFICIENCY IN PARKINSON’S DISEASE. Lancet. 1989;333(8649):1269.
Mizuno Y, Ohta S, Tanaka M, Takamiya S, Suzuki K, Sato T, Oya H, Ozawa T, Kagawa Y. Deficiencies in complex I subunits of the respiratory chain in Parkinson’s disease. Biochem Biophys Res Commun. 1989;163(3):1450–5.
Keeney PM, Xie J, Capaldi RA, Bennett JP Jr. Parkinson’s disease brain mitochondrial complex I has oxidatively damaged subunits and is functionally impaired and misassembled. J Neurosci. 2006;26(19):5256–64.
Toomey CE, Heywood WE, Evans JR, Lachica J, Pressey SN, Foti SC, Al Shahrani M, D’Sa K, Hargreaves IP, Heales S, et al. Mitochondrial dysfunction is a key pathological driver of early stage Parkinson’s. Acta Neuropathol Commun. 2022;10(1):134.
Chen C, McDonald D, Blain A, Mossman E, Atkin K, Marusich MF, Capaldi R, Bone L, Smith A, Filby A, et al. Parkinson’s disease neurons exhibit alterations in mitochondrial quality control proteins. Npj Parkinson’s Disease. 2023;9(1):120.
Pacelli C, Giguère N, Bourque MJ, Lévesque M, Slack RS, Trudeau L. Elevated mitochondrial bioenergetics and axonal arborization size are key contributors to the vulnerability of dopamine neurons. Curr Biol. 2015;25(18):2349–60.
Haddad D, Nakamura K. Understanding the susceptibility of dopamine neurons to mitochondrial stressors in Parkinson’s disease. FEBS Lett. 2015;589(24 Pt A):3702–13.
Surmeier DJ. Determinants of dopaminergic neuron loss in Parkinson’s disease. Febs j. 2018;285(19):3657–68.
Meiser J, Weindl D, Hiller K. Complexity of dopamine metabolism. Cell Communication Signal. 2013;11(1):34.
Helley MP, Pinnell J, Sportelli C, Tieu K. Mitochondria: a common target for genetic mutations and environmental toxicants in Parkinson’s Disease. Front Genet. 2017;8:177.
Li W, Fu Y, Halliday GM, Sue CM. PARK genes Link mitochondrial dysfunction and alpha-Synuclein Pathology in sporadic Parkinson’s Disease. Front Cell Dev Biol. 2021;9:612476.
Mitochondrial Dysfunction in Dopaminergic Neurons Derived from Patients with LRRK2-and SNCA-Associated Genetic Forms of Parkinson’s Disease. Curr Issues Mol Biol 2023, 45(10):8395–8411.
Park J-S, Davis RL, Sue CM. Mitochondrial dysfunction in Parkinson’s Disease: new mechanistic insights and therapeutic perspectives. Curr Neurol Neurosci Rep. 2018;18(5):21–21.
Zimprich A, Biskup S, Leitner P, Lichtner P, Farrer M, Lincoln S, Kachergus J, Hulihan M, Uitti RJ, Calne DB, et al. Mutations in LRRK2 cause autosomal-dominant parkinsonism with pleomorphic pathology. Neuron. 2004;44(4):601–7.
Singh A, Zhi L, Zhang H. LRRK2 and mitochondria: recent advances and current views. Brain Res. 2019;1702:96–104.
Pickrell AM, Youle RJ. The roles of PINK1, parkin, and mitochondrial fidelity in Parkinson’s disease. Neuron. 2015;85(2):257–73.
Ge P, Dawson VL, Dawson TM. PINK1 and Parkin mitochondrial quality control: a source of regional vulnerability in Parkinson’s disease. Mol Neurodegener. 2020;15(1):20.
Davis GC, Williams AC, Markey SP, Ebert MH, Caine ED, Reichert CM, Kopin IJ. Chronic parkinsonism secondary to intravenous injection of meperidine analogues. Psychiatry Res. 1979;1(3):249–54.
Langston JW, Ballard P, Tetrud JW, Irwin I. Chronic parkinsonism in humans due to a product of meperidine-analog synthesis. Science. 1983;219(4587):979–80.
Spivey A. Rotenone and paraquat linked to Parkinson’s disease: human exposure study supports years of animal studies. Environ Health Perspect. 2011;119(6):A259–259.
Tanner CM, Kamel F, Ross GW, Hoppin JA, Goldman SM, Korell M, Marras C, Bhudhikanok GS, Kasten M, Chade AR, et al. Rotenone, paraquat, and Parkinson’s disease. Environ Health Perspect. 2011;119(6):866–72.
Pezzoli G, Cereda E. Exposure to pesticides or solvents and risk of Parkinson disease. Neurology. 2013;80(22):2035–41.
Huang M, Bargues-Carot A, Riaz Z, Wickham H, Zenitsky G, Jin H, Anantharam V, Kanthasamy A, Kanthasamy AG. Impact of Environmental Risk Factors on Mitochondrial Dysfunction, Neuroinflammation, Protein Misfolding, and Oxidative Stress in the Etiopathogenesis of Parkinson’s Disease. Int J Mol Sci 2022, 23(18).
Slézia A, Hegedüs P, Rusina E, Lengyel K, Solari N, Kaszas A, Balázsfi D, Botzanowski B, Acerbo E, Missey F, et al. Behavioral, neural and ultrastructural alterations in a graded-dose 6-OHDA mouse model of early-stage Parkinson’s disease. Sci Rep. 2023;13(1):19478.
Pyatha S, Kim H, Lee D, Kim K. Association between Heavy Metal Exposure and Parkinson’s Disease: A Review of the Mechanisms Related to Oxidative Stress. Antioxid (Basel) 2022, 11(12).
Reeve A, Simcox E, Turnbull D. Ageing and Parkinson’s disease: why is advancing age the biggest risk factor? Ageing Res Rev. 2014;14(100):19–30.
Ludtmann MH, Angelova PR, Ninkina NN, Gandhi S, Buchman VL, Abramov AY. Monomeric Alpha-Synuclein exerts a physiological role on Brain ATP synthase. J Neurosci. 2016;36(41):10510–21.
Norris KL, Hao R, Chen LF, Lai CH, Kapur M, Shaughnessy PJ, Chou D, Yan J, Taylor JP, Engelender S, et al. Convergence of Parkin, PINK1, and α-Synuclein on stress-induced mitochondrial morphological remodeling. J Biol Chem. 2015;290(22):13862–74.
Devi L, Raghavendran V, Prabhu BM, Avadhani NG, Anandatheerthavarada HK. Mitochondrial Import and Accumulation of α-Synuclein impair complex I in human dopaminergic neuronal cultures and Parkinson Disease Brain*. J Biol Chem. 2008;283(14):9089–100.
Ludtmann MHR, Angelova PR, Horrocks MH, Choi ML, Rodrigues M, Baev AY, Berezhnov AV, Yao Z, Little D, Banushi B, et al. : α-synuclein oligomers interact with ATP synthase and open the permeability transition pore in Parkinson’s disease. Nat Commun. 2018;9(1):2293.
Esteves AR, Arduíno DM, Silva DF, Oliveira CR, Cardoso SM. Mitochondrial dysfunction: the Road to Alpha-Synuclein oligomerization in PD. Parkinsons Dis. 2011;2011:693761.
Choi ML, Chappard A, Singh BP, Maclachlan C, Rodrigues M, Fedotova EI, Berezhnov AV, De S, Peddie CJ, Athauda D, et al. Pathological structural conversion of α-synuclein at the mitochondria induces neuronal toxicity. Nat Neurosci. 2022;25(9):1134–48.
Lurette O, Martín-Jiménez R, Khan M, Sheta R, Jean S, Schofield M, Teixeira M, Rodriguez-Aller R, Perron I, Oueslati A, et al. Aggregation of alpha-synuclein disrupts mitochondrial metabolism and induce mitophagy via cardiolipin externalization. Cell Death Dis. 2023;14(11):729.
Schildknecht S, Gerding HR, Karreman C, Drescher M, Lashuel HA, Outeiro TF, Di Monte DA, Leist M. Oxidative and nitrative alpha-synuclein modifications and proteostatic stress: implications for disease mechanisms and interventions in synucleinopathies. J Neurochem. 2013;125(4):491–511.
Li H-Y, Liu D-S, Zhang Y-B, Rong H, Zhang X-J. The interaction between alpha-synuclein and mitochondrial dysfunction in Parkinson’s disease. Biophys Chem. 2023;303:107122.
Dias V, Junn E, Mouradian MM. The role of oxidative stress in Parkinson’s disease. J Parkinsons Dis. 2013;3(4):461–91.
Alam ZI, Jenner A, Daniel SE, Lees AJ, Cairns N, Marsden CD, Jenner P, Halliwell B. Oxidative DNA damage in the parkinsonian brain: an apparent selective increase in 8-hydroxyguanine levels in substantia nigra. J Neurochem. 1997;69(3):1196–203.
Chalovich EM, Zhu J-h, Caltagarone J, Bowser R, Chu CT. Functional repression of cAMP response element in 6-Hydroxydopamine-treated neuronal cells. J Biol Chem. 2006;281(26):17870–81.
Sakamoto K, Karelina K, Obrietan K. CREB: a multifaceted regulator of neuronal plasticity and protection. J Neurochem. 2011;116(1):1–9.
Zhu JH, Kulich SM, Oury TD, Chu CT. Cytoplasmic aggregates of phosphorylated extracellular signal-regulated protein kinases in Lewy body diseases. Am J Pathol. 2002;161(6):2087–98.
Ferrer I, Blanco R, Carmona M, Puig B, Barrachina M, Gómez C, Ambrosio S. Active, phosphorylation-dependent mitogen-activated protein kinase (MAPK/ERK), stress-activated protein kinase/c-Jun N-terminal kinase (SAPK/JNK), and p38 kinase expression in Parkinson’s disease and dementia with Lewy bodies. J Neural Transm (Vienna). 2001;108(12):1383–96.
Dagda RK, Zhu J, Kulich SM, Chu CT. Mitochondrially localized ERK2 regulates mitophagy and autophagic cell stress: implications for Parkinson’s disease. Autophagy. 2008;4(6):770–82.
Maeder CI, Kim J-I, Liang X, Kaganovsky K, Shen A, Li Q, Li Z, Wang S, Xu XZS, Li JB, et al. The THO complex coordinates transcripts for Synapse Development and dopamine neuron survival. Cell. 2018;174(6):1436–e14491420.
Bitetto G, Di Fonzo A. Nucleo–cytoplasmic transport defects and protein aggregates in neurodegeneration. Translational Neurodegeneration. 2020;9(1):1–16.
Goers J, Manning-Bog AB, McCormack AL, Millett IS, Doniach S, Di Monte DA, Uversky VN, Fink AL. Nuclear localization of alpha-synuclein and its interaction with histones. Biochemistry. 2003;42(28):8465–71.
Zhou M, Xu S, Mi J, Uéda K, Chan P. Nuclear translocation of alpha-synuclein increases susceptibility of MES23.5 cells to oxidative stress. Brain Res. 2013;1500:19–27.
Koss DJ, Erskine D, Porter A, Palmoski P, Menon H, Todd OGJ, Leite M, Attems J, Outeiro TF. Nuclear alpha-synuclein is present in the human brain and is modified in dementia with Lewy bodies. Acta Neuropathol Commun. 2022;10(1):98.
Pinho R, Paiva I, Jercic KG, Fonseca-Ornelas L, Gerhardt E, Fahlbusch C, Garcia-Esparcia P, Kerimoglu C, Pavlou MAS, Villar-Piqué A, et al. Nuclear localization and phosphorylation modulate pathological effects of alpha-synuclein. Hum Mol Genet. 2019;28(1):31–50.
Siddiqui A, Chinta SJ, Mallajosyula JK, Rajagopolan S, Hanson I, Rane A, Melov S, Andersen JK. Selective binding of nuclear alpha-synuclein to the PGC1alpha promoter under conditions of oxidative stress may contribute to losses in mitochondrial function: implications for Parkinson’s disease. Free Radic Biol Med. 2012;53(4):993–1003.
Pasha T, Zatorska A, Sharipov D, Rogelj B, Hortobágyi T, Hirth F. Karyopherin abnormalities in neurodegenerative proteinopathies. Brain. 2021;144(10):2915–32.
Geertsma HM, Suk TR, Ricke KM, Horsthuis K, Parmasad J-LA, Fisk ZA, Callaghan SM, Rousseaux MWC. Constitutive nuclear accumulation of endogenous alpha-synuclein in mice causes motor impairment and cortical dysfunction, independent of protein aggregation. Hum Mol Genet. 2022;31(21):3613–28.
Schell H, Hasegawa T, Neumann M, Kahle PJ. Nuclear and neuritic distribution of serine-129 phosphorylated alpha-synuclein in transgenic mice. Neuroscience. 2009;160(4):796–804.
Chen V, Moncalvo M, Tringali D, Tagliafierro L, Shriskanda A, Ilich E, Dong W, Kantor B, Chiba-Falek O. The mechanistic role of alpha-synuclein in the nucleus: impaired nuclear function caused by familial Parkinson’s disease SNCA mutations. Hum Mol Genet. 2020;29(18):3107–21.
Rousseaux MW, de Haro M, Lasagna-Reeves CA, De Maio A, Park J, Jafar-Nejad P, Al-Ramahi I, Sharma A, See L, Lu N et al. TRIM28 regulates the nuclear accumulation and toxicity of both alpha-synuclein and tau. Elife 2016, 5.
Ma K-L, Song L-K, Yuan Y-H, Zhang Y, Han N, Gao K, Chen N-H. The nuclear accumulation of alpha-synuclein is mediated by importin alpha and promotes neurotoxicity by accelerating the cell cycle. Neuropharmacology. 2014;82:132–42.
Tagliafierro L, Zamora ME, Chiba-Falek O. Multiplication of the SNCA locus exacerbates neuronal nuclear aging. Hum Mol Genet. 2019;28(3):407–21.
Liu GH, Qu J, Suzuki K, Nivet E, Li M, Montserrat N, Yi F, Xu X, Ruiz S, Zhang W, et al. Progressive degeneration of human neural stem cells caused by pathogenic LRRK2. Nature. 2012;491(7425):603–7.
Shani V, Safory H, Szargel R, Wang N, Cohen T, Elghani FA, Hamza H, Savyon M, Radzishevsky I, Shaulov L, et al. Physiological and pathological roles of LRRK2 in the nuclear envelope integrity. Hum Mol Genet. 2019;28(23):3982–96.
Tsika E, Kannan M, Foo CS, Dikeman D, Glauser L, Gellhaar S, Galter D, Knott GW, Dawson TM, Dawson VL, et al. Conditional expression of Parkinson’s disease-related R1441C LRRK2 in midbrain dopaminergic neurons of mice causes nuclear abnormalities without neurodegeneration. Neurobiol Dis. 2014;71:345–58.
Um JW, Min DS, Rhim H, Kim J, Paik SR, Chung KC. Parkin Ubiquitinates and promotes the degradation of RanBP2*. J Biol Chem. 2006;281(6):3595–603.
Cho K-i, Searle K, Webb M, Yi H, Ferreira PA. Ranbp2 haploinsufficiency mediates distinct cellular and biochemical phenotypes in brain and retinal dopaminergic and glia cells elicited by the parkinsonian neurotoxin, 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP). Cell Mol Life Sci. 2012;69(20):3511–27.
Krisko A, Radman M. Protein damage, ageing and age-related diseases. Open Biol. 2019;9(3):180249.
Reeg S, Grune T. Protein oxidation in aging: does it play a role in aging progression? Antioxid Redox Signal. 2015;23(3):239–55.
Kristiani L, Kim Y. The interplay between oxidative stress and the Nuclear Lamina contributes to Laminopathies and Age-Related diseases. In: Cells 12; 2023.
Heo J. Redox regulation of Ran GTPase. Biochem Biophys Res Commun. 2008;376(3):568–72.
Chatterjee M, Paschal BM. Disruption of the ran system by Cysteine Oxidation of the Nucleotide Exchange factor RCC1. Mol Cell Biol. 2015;35(3):566–81.
Kodiha M, Chu A, Matusiewicz N, Stochaj U. Multiple mechanisms promote the inhibition of classical nuclear import upon exposure to severe oxidative stress. Cell Death Differ. 2004;11(8):862–74.
Datta S, Snow CJ, Paschal BM. A pathway linking oxidative stress and the ran GTPase system in progeria. Mol Biol Cell. 2014;25(8):1202–15.
Kodiha M, Tran D, Qian C, Morogan A, Presley JF, Brown CM, Stochaj U. Oxidative stress mislocalizes and retains transport factor importin-α and nucleoporins Nup153 and Nup88 in nuclei where they generate high molecular mass complexes. Biochim et Biophys Acta (BBA) – Mol Cell Res. 2008;1783(3):405–18.
Crampton N, Kodiha M, Shrivastava S, Umar R, Stochaj U. Oxidative stress inhibits nuclear protein export by multiple mechanisms that target FG nucleoporins and Crm1. Mol Biol Cell. 2009;20(24):5106–16.
Kodiha M, Stochaj U. Nuclear transport: a switch for the oxidative stress-signaling circuit? J Signal Transduct. 2012, 2012:208650.
Mahboubi H, Seganathy E, Kong D, Stochaj U. Identification of novel stress Granule Components that are involved in Nuclear Transport. PLoS ONE. 2013;8(6):e68356.
Mizuguchi-Hata C, Ogawa Y, Oka M, Yoneda Y. Quantitative regulation of nuclear pore complex proteins by O-GlcNAcylation. Biochim Biophys Acta. 2013;1833(12):2682–9.
Kosako H, Imamoto N. Phosphorylation of nucleoporins: signal transduction-mediated regulation of their interaction with nuclear transport receptors. Nucleus (Austin Tex). 2010;1(4):309–13.
Faustino RS, Maddaford TG, Pierce GN. Mitogen activated protein kinase at the nuclear pore complex. J Cell Mol Med. 2011;15(4):928–37.
Kodiha M, Bański P, Stochaj U. Interplay between MEK and PI3 kinase signaling regulates the subcellular localization of protein kinases ERK1/2 and akt upon oxidative stress. FEBS Lett. 2009;583(12):1987–93.
Zachara NE, O’Donnell N, Cheung WD, Mercer JJ, Marth JD, Hart GW. Dynamic O-GlcNAc modification of Nucleocytoplasmic Proteins in response to stress: a SURVIVAL RESPONSE OF MAMMALIAN CELLS*. J Biol Chem. 2004;279(29):30133–42.
Kátai E, Pál J, Poór VS, Purewal R, Miseta A, Nagy T. Oxidative stress induces transient O-GlcNAc elevation and tau dephosphorylation in SH-SY5Y cells. J Cell Mol Med. 2016;20(12):2269–77.
Kodiha M, Tran D, Morogan A, Qian C, Stochaj U. Dissecting the signaling events that impact classical nuclear import and target nuclear transport factors. PLoS ONE. 2009;4(12):e8420.
Lee BE, Kim HY, Kim HJ, Jeong H, Kim BG, Lee HE, Lee J, Kim HB, Lee SE, Yang YR, et al. O-GlcNAcylation regulates dopamine neuron function, survival and degeneration in Parkinson disease. Brain. 2020;143(12):3699–716.
Tavassoly O, Yue J, Vocadlo DJ. Pharmacological inhibition and knockdown of O-GlcNAcase reduces cellular internalization of α-synuclein preformed fibrils. Febs j. 2021;288(2):452–70.
Levine PM, Galesic A, Balana AT, Mahul-Mellier AL, Navarro MX, De Leon CA, Lashuel HA, Pratt MR. α-Synuclein O-GlcNAcylation alters aggregation and toxicity, revealing certain residues as potential inhibitors of Parkinson’s disease. Proc Natl Acad Sci U S A. 2019;116(5):1511–9.
Hart GW, Housley MP, Slawson C. Cycling of O-linked β-N-acetylglucosamine on nucleocytoplasmic proteins. Nature. 2007;446(7139):1017–22.
Coyne AN, Rothstein JD. Nuclear pore complexes — a doorway to neural injury in neurodegeneration. Nat Reviews Neurol. 2022;18(6):348–62.
Masrori P, Van Damme P. Amyotrophic lateral sclerosis: a clinical review. Eur J Neurol. 2020;27(10):1918–29.
Zhang J, Ito H, Wate R, Ohnishi S, Nakano S, Kusaka H. Altered distributions of nucleocytoplasmic transport-related proteins in the spinal cord of a mouse model of amyotrophic lateral sclerosis. Acta Neuropathol. 2006;112(6):673–80.
Jovičić A, Mertens J, Boeynaems S, Bogaert E, Chai N, Yamada SB, Paul JW, Sun S, Herdy JR, Bieri G, et al. Modifiers of C9orf72 dipeptide repeat toxicity connect nucleocytoplasmic transport defects to FTD/ALS. Nat Neurosci. 2015;18(9):1226–9.
Zhang K, Donnelly CJ, Haeusler AR, Grima JC, Machamer JB, Steinwald P, Daley EL, Miller SJ, Cunningham KM, Vidensky S, et al. The C9orf72 repeat expansion disrupts nucleocytoplasmic transport. Nature. 2015;525(7567):56–61.
Freibaum BD, Lu Y, Lopez-Gonzalez R, Kim NC, Almeida S, Lee K-H, Badders N, Valentine M, Miller BL, Wong PC, et al. GGGGCC repeat expansion in C9orf72 compromises nucleocytoplasmic transport. Nature. 2015;525(7567):129–33.
Coyne AN, Baskerville V, Zaepfel BL, Dickson DW, Rigo F, Bennett F, Lusk CP, Rothstein JD. Nuclear accumulation of CHMP7 initiates nuclear pore complex injury and subsequent TDP-43 dysfunction in sporadic and familial ALS. Sci Transl Med. 2021, 13(604).
Chou C-C, Zhang Y, Umoh ME, Vaughan SW, Lorenzini I, Liu F, Sayegh M, Donlin-Asp PG, Chen YH, Duong DM, et al. TDP-43 pathology disrupts nuclear pore complexes and nucleocytoplasmic transport in ALS/FTD. Nat Neurosci. 2018;21(2):228–39.
Giampetruzzi A, Danielson EW, Gumina V, Jeon M, Boopathy S, Brown RH, Ratti A, Landers JE, Fallini C. Modulation of actin polymerization affects nucleocytoplasmic transport in multiple forms of amyotrophic lateral sclerosis. Nat Commun. 2019;10(1):3827.
Shang J, Yamashita T, Nakano Y, Morihara R, Li X, Feng T, Liu X, Huang Y, Fukui Y, Hishikawa N, et al. Aberrant distributions of nuclear pore complex proteins in ALS mice and ALS patients. Neuroscience. 2017;350:158–68.
Trist BG, Hilton JB, Hare DJ, Crouch PJ, Double KL. Superoxide dismutase 1 in Health and Disease: how a Frontline antioxidant becomes neurotoxic. Angew Chem Int Ed Engl. 2021;60(17):9215–46.
Erkkinen MG, Kim MO, Geschwind MD. Clinical neurology and epidemiology of the Major Neurodegenerative diseases. Cold Spring Harb Perspect Biol 2018, 10(4).
Twohig D, Nielsen HM. α-synuclein in the pathophysiology of Alzheimer’s disease. Mol Neurodegener. 2019;14(1):23.
Eftekharzadeh B, Daigle JG, Kapinos LE, Coyne A, Schiantarelli J, Carlomagno Y, Cook C, Miller SJ, Dujardin S, Amaral AS, et al. Tau protein disrupts nucleocytoplasmic transport in Alzheimer’s Disease. Neuron. 2018;99(5):925–e940927.
Zhang X, Gao F, Wang D, Li C, Fu Y, He W, Zhang J. Tau Pathology in Parkinson’s Disease. Front Neurol. 2018;9:809.
Leone L, Colussi C, Gironi K, Longo V, Fusco S, Li Puma DD, D’Ascenzo M, Grassi C. Altered Nup153 expression impairs the function of cultured hippocampal neural stem cells isolated from a mouse model of Alzheimer’s Disease. Mol Neurobiol. 2019;56(8):5934–49.
Malik SC, Lin JD, Ziegler-Waldkirch S, Tholen S, Deshpande SS, Schwabenland M, Schilling O, Vlachos A, Meyer-Luehmann M, Schachtrup C. Tpr Misregulation in Hippocampal Neural Stem Cells in Mouse Models of Alzheimer’s Disease. Cells 2023, 12(23).
Lee BE, Suh P-G, Kim J-I. O-GlcNAcylation in health and neurodegenerative diseases. Exp Mol Med. 2021;53(11):1674–82.
Grima JC, Daigle JG, Arbez N, Cunningham KC, Zhang K, Ochaba J, Geater C, Morozko E, Stocksdale J, Glatzer JC, et al. Mutant huntingtin disrupts the Nuclear Pore Complex. Neuron. 2017;94(1):93–e107106.
Flokas ME, Tomani M, Agdere L, Brown B. Triple A syndrome (Allgrove syndrome): improving outcomes with a multidisciplinary approach. Pediatr Health Med Ther. 2019;10:99–106.
Cronshaw JM, Matunis MJ. The nuclear pore complex protein ALADIN is mislocalized in triple A syndrome. Proc Natl Acad Sci U S A. 2003;100(10):5823–7.
Storr HL, Kind B, Parfitt DA, Chapple JP, Lorenz M, Koehler K, Huebner A, Clark AJ. Deficiency of ferritin heavy-chain nuclear import in triple a syndrome implies nuclear oxidative damage as the primary disease mechanism. Mol Endocrinol. 2009;23(12):2086–94.
Hirano M, Furiya Y, Asai H, Yasui A, Ueno S. ALADIN I482S causes selective failure of nuclear protein import and hypersensitivity to oxidative stress in triple A syndrome. Proc Natl Acad Sci. 2006;103(7):2298–303.
Tsai YL, Coady TH, Lu L, Zheng D, Alland I, Tian B, Shneider NA, Manley JL. ALS/FTD-associated protein FUS induces mitochondrial dysfunction by preferentially sequestering respiratory chain complex mRNAs. Genes Dev. 2020;34(11–12):785–805.
Teyssou E, Chartier L, Roussel D, Perera ND, Nemazanyy I, Langui D, Albert M, Larmonier T, Saker S, Salachas F et al. The amyotrophic lateral sclerosis M114T PFN1 mutation deregulates alternative Autophagy pathways and mitochondrial homeostasis. Int J Mol Sci 2022, 23(10).
Ganjam GK, Bolte K, Matschke LA, Neitemeier S, Dolga AM, Höllerhage M, Höglinger GU, Adamczyk A, Decher N, Oertel WH, et al. Mitochondrial damage by α-synuclein causes cell death in human dopaminergic neurons. Cell Death Dis. 2019;10(11):865.
Delcambre S, Ghelfi J, Ouzren N, Grandmougin L, Delbrouck C, Seibler P, Wasner K, Aasly JO, Klein C, Trinh J et al. Mitochondrial mechanisms of LRRK2 G2019S Penetrance. Front Neurol 2020, 11.
Get the source article here

