A newly identified brain network may be the real driver of Parkinson’s—and precisely targeting it just delivered a major boost in symptom relief.
Parkinson’s disease is a progressive neurological condition that affects more than 1 million people in the United States and over 10 million worldwide. It causes a wide range of disabling symptoms, including tremors, difficulty with movement, sleep problems, and declines in thinking and memory. Existing treatments such as long-term drug therapy and invasive deep brain stimulation (DBS) can ease symptoms, but they do not stop the disease from worsening or provide a cure.
A New Brain Network Linked to Parkinson’s
An international research team led by China’s Changping Laboratory, working with Washington University School of Medicine in St. Louis and other institutions, has identified a specific brain region tied to the central problems of Parkinson’s disease. The scientists focused on a brain network known as the somato-cognitive action network (SCAN). When this network was targeted using a non-invasive experimental approach called transcranial magnetic stimulation (TMS), patients experienced more than twice the symptom improvement seen when nearby brain regions were stimulated instead.
The findings, published today (February 4) in Nature, reshape how scientists understand the neurological basis of Parkinson’s disease and point toward more precise and potentially more effective treatment strategies.
“This work demonstrates that Parkinson’s is a SCAN disorder, and the data strongly suggest that if you target the SCAN in a personalized, precise manner you can treat Parkinson’s more successfully than was previously possible,” said co-author Nico U. Dosenbach, MD, PhD, the David M. & Tracy S. Holtzman Professor of Neurology at WashU Medicine. “Changing the activity within SCAN could slow or reverse the progression of the disease, not just treat the symptoms.”
Understanding the Role of SCAN
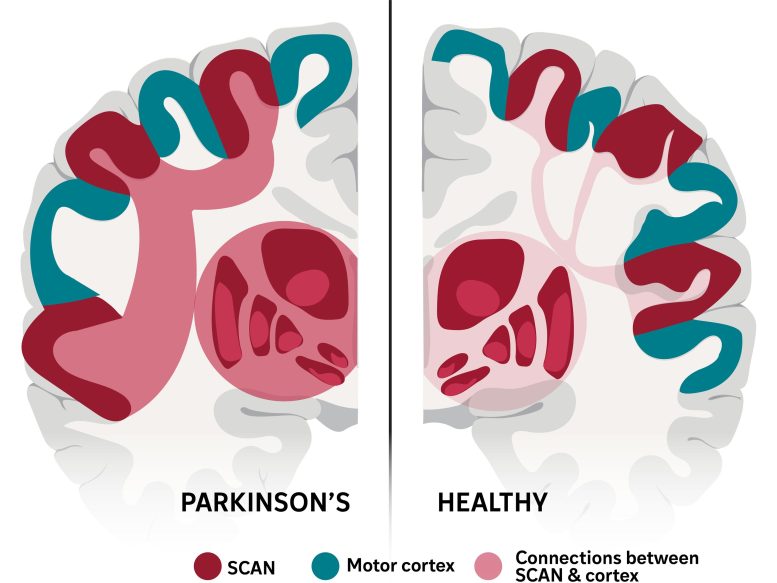
Dosenbach first described the SCAN in Nature in 2023. This network sits within the motor cortex, the area of the brain that controls voluntary movement, and helps translate plans for action into physical motion while monitoring how those actions unfold. Because Parkinson’s disease affects far more than movement alone, influencing digestion, sleep, motivation, and cognition, senior author Hesheng Liu, PhD, partnered with Dosenbach to investigate whether problems within SCAN could explain the disease’s wide-ranging symptoms and offer a new treatment target.
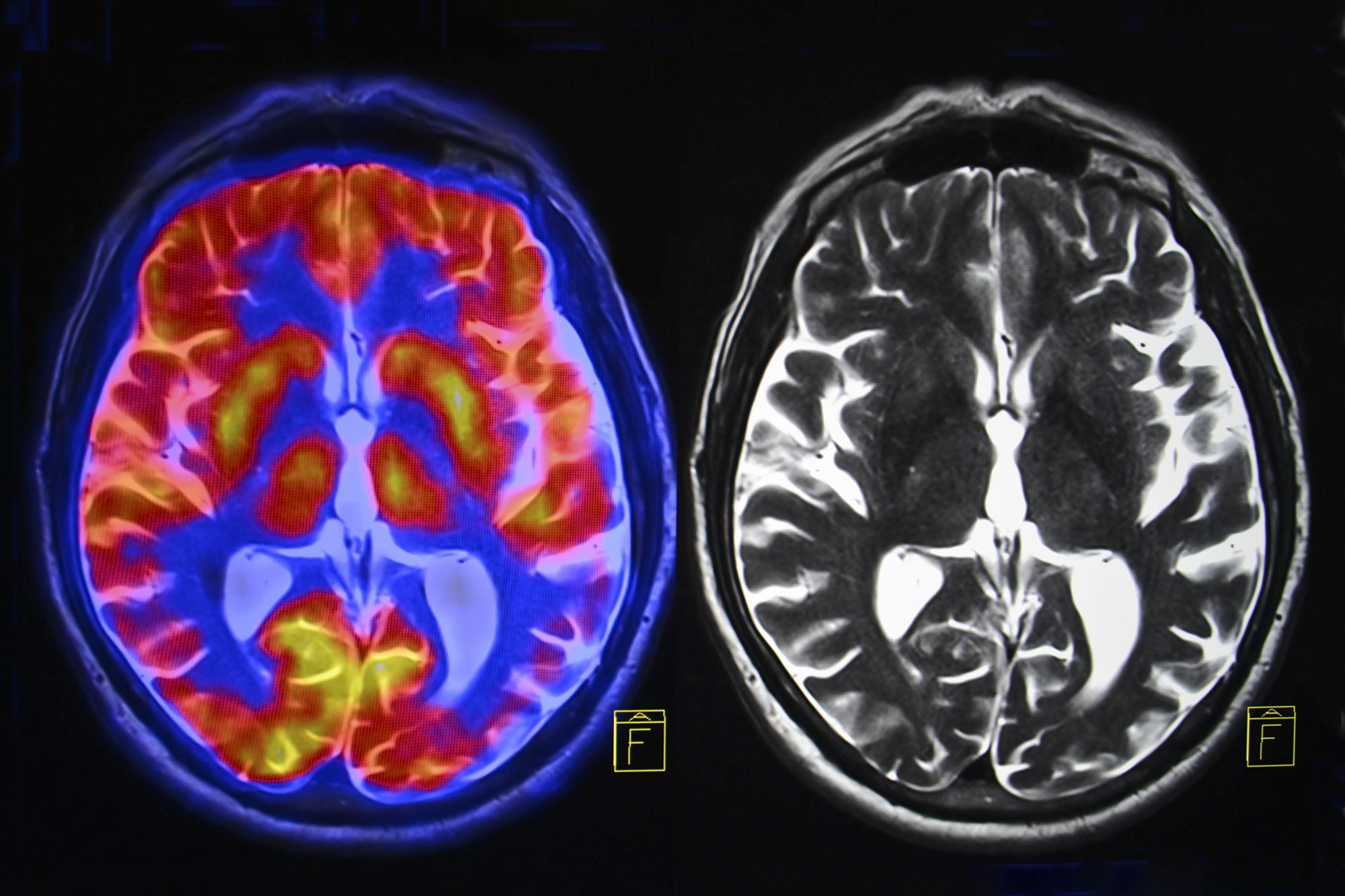
To explore this idea, Liu’s team analyzed multiple types of brain imaging data from more than 800 participants in the United States and China. The study included people with Parkinson’s disease receiving DBS or non-invasive therapies such as transcranial magnetic stimulation, focused ultrasound stimulation, and medications. Healthy volunteers and individuals with other movement disorders were also included for comparison.
Abnormal Brain Connectivity Identified
The researchers found that Parkinson’s disease is marked by unusually strong connections between the SCAN and the subcortex, a brain region involved in emotion, memory, and motor control. Across all four treatments examined in the study, the therapies worked best when they reduced this excessive connectivity. Doing so helped restore more normal activity in the brain circuit responsible for planning and coordinating actions.
“For decades, Parkinson’s has been primarily associated with motor deficits and the basal ganglia,” the part of the brain that controls muscle movements, Liu said. “Our work shows that the disease is rooted in a much broader network dysfunction. The SCAN is hyperconnected to key regions associated with Parkinson’s disease, and this abnormal wiring disrupts not only movement but also related cognitive and bodily functions.”
Precision Treatment Shows Promise
Using these insights, the researchers developed a precision treatment system designed to target the SCAN without surgery and with millimeter-level accuracy. They used transcranial magnetic stimulation, which delivers magnetic pulses to the brain through a device placed on the scalp. In a clinical trial, 18 patients who received SCAN-targeted stimulation showed a 56% response rate after two weeks. By comparison, only 22% of 18 patients who received stimulation to nearby brain areas improved, representing a 2.5-fold increase in effectiveness.
“With non-invasive treatments, we could start treating with neuromodulation much earlier than is currently done with DBS” because they don’t require brain surgery, Dosenbach said.
He noted that additional basic research is still needed to determine how different parts of the SCAN contribute to specific Parkinson’s symptoms.
Looking ahead, Dosenbach plans to lead clinical trials with Turing Medical, a WashU Medicine startup he co-founded. These studies will test a non-invasive therapy that uses surface electrode strips placed over SCAN regions to improve walking difficulties in people with Parkinson’s disease. He also intends to explore low-intensity focused ultrasound as another non-invasive method for adjusting SCAN activity using acoustic energy.
Reference: “Parkinson’s disease as a somato-cognitive action network disorder” by Ren J, Zhang W, Dahmani L, Gordon EM, Li S, Zhou Y, Long Y, Huang J, Zhu Y, Guo N, Jiang C, Zhang F, Bai Y, Wei W, Wu Y, Bush A, Vissani M, Wei L, Oehrn CR, Morrison MA, Zhu Y, Zhang C, Hu Q, Yin Y, Cui W, Fu X, Zhang P, Wang W, Ji GJ, Wang K, Wang Z, Kimberley T, Little S, Starr PA, Richardson RM, Li L, Wang M, Wang D, Dosenbach NUF, Liu H., 4 February 2026, Nature.
DOI: 10.1038/s41586-025-10059-1
This work was supported by the Changping Laboratory, the U.S. National Institutes of Health (MH096773, MH122066, MH121276, MH124567, NS129521, NS088590, R01NS131405, U01NS098969, and U01NS117836), the National Natural Science Foundation of China (81527901, 81720108021, 81971689, 31970979, and 82090034), the National Key R&D Program of China (2017YFE0103600), the Intellectual and Developmental Disabilities Research Center; the Kiwanis Foundation; the Washington University Hope Center for Neurological Disorders; and the Collaborative Innovation Center of Neuropsychiatric Disorders and Mental Health of Anhui Province (2020xkjT05). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
H.L. is the chief scientist of Neural Galaxy Inc. L.L. serves on the scientific advisory board for Beijing Pins Medical Co., Ltd and are listed as inventors in issued patents and patent applications on the deep brain stimulator used in this work. N.U.F.D. has a financial interest in Turing Medical Inc. and may financially benefit if the company is successful in marketing FIRMM motion monitoring software or BullsAI neuromodulation targeting software or PACE neuromodulation systems. E.M.G. and N.U.F.D. may receive royalty income based on FIRMM technology developed at Washington University School of Medicine and licensed to Turing Medical Inc. N.U.F.D. is a co-founder of Turing Medical Inc. These potential conflicts of interest have been reviewed and are managed by Washington University School of Medicine. S.L. consults for Iota Biosciences. P.A.S. receives support from Medtronic and Boston Scientific for fellowship education.
Never miss a breakthrough: Join the SciTechDaily newsletter.
Follow us on Google and Google News.
This was shown first on: https://scitechdaily.com/scientists-may-have-found-the-true-source-of-parkinsons-disease/