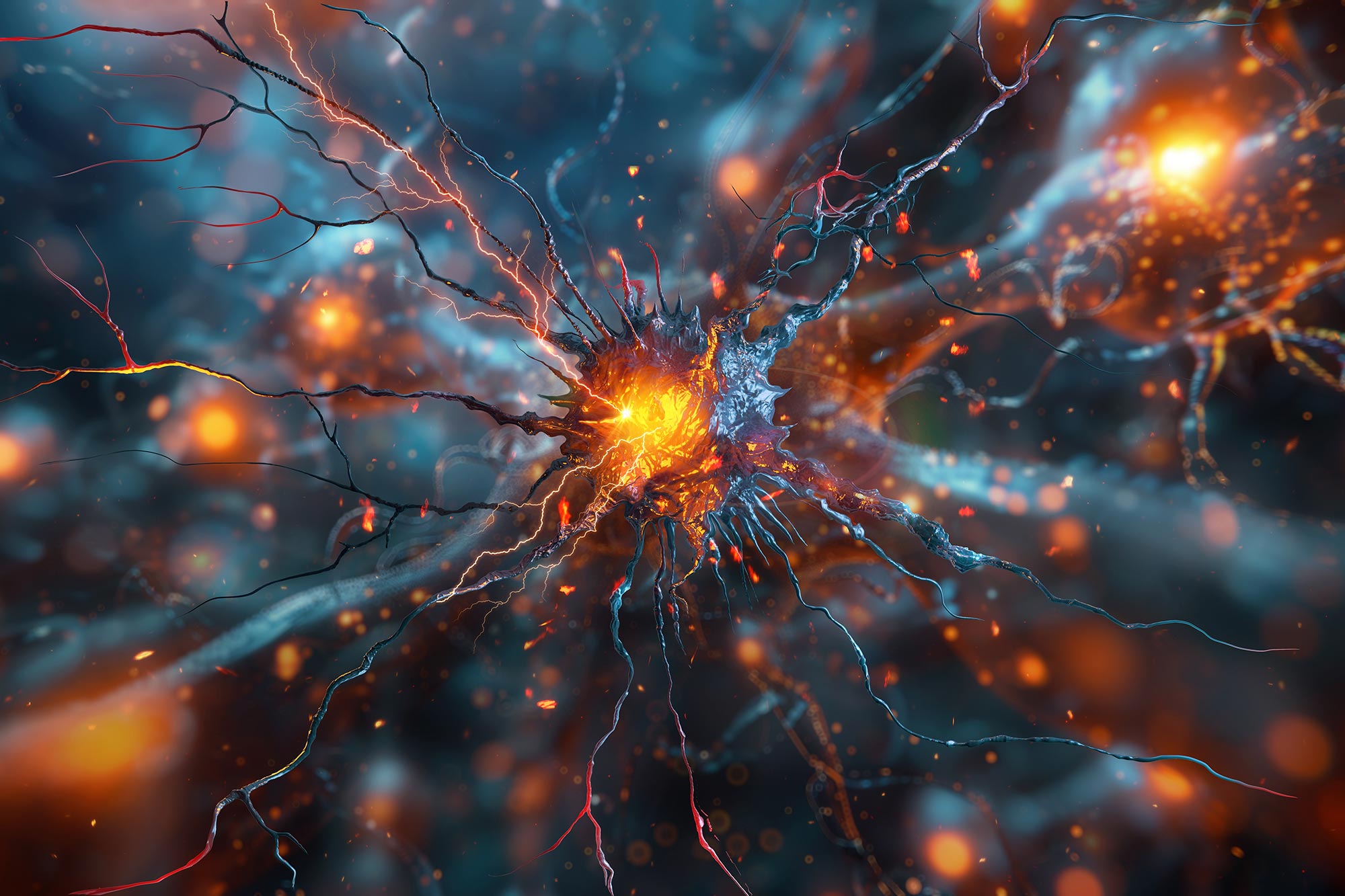
A groundbreaking imaging technique has, for the first time, made the invisible visible.
For the first time, scientists have managed to directly observe and measure the protein clusters thought to spark the onset of Parkinson’s disease, representing a major leap forward in understanding this rapidly growing neurological disorder.
These microscopic structures, known as alpha-synuclein oligomers, have long been suspected of initiating the disease within the brain. However, until now, researchers had been unable to detect them directly in human brain tissue.
A team from the University of Cambridge, UCL, the Francis Crick Institute, and Polytechnique Montréal has now developed an advanced imaging method that enables them to visualize, count, and compare these elusive clusters. One of the researchers described the breakthrough as being “like being able to see stars in broad daylight.”
The findings, published in Nature Biomedical Engineering, could reveal new details about how Parkinson’s spreads through the brain and aid in the development of early diagnostic tools and future treatments.
Currently, around 166,000 people in the UK live with Parkinson’s disease, and that number continues to grow. Globally, the total is expected to reach 25 million by 2050. While existing medications can ease symptoms such as tremors and muscle stiffness, there are still no treatments capable of slowing or stopping the progression of the disease itself.
From Lewy Bodies to Oligomers
For more than a century, doctors have recognized Parkinson’s by the presence of large protein deposits called Lewy bodies. But scientists have suspected that smaller, earlier-forming oligomers may cause the damage to brain cells. Until now, these oligomers were simply too small to see – just a few nanometers long.
“Lewy bodies are the hallmark of Parkinson’s, but they essentially tell you where the disease has been, not where it is right now,” said Professor Steven Lee from Cambridge’s Yusuf Hamied Department of Chemistry, who co-led the research. “If we can observe Parkinson’s at its earliest stages, that would tell us a whole lot more about how the disease develops in the brain and how we might be able to treat it.”
Now, Lee and his colleagues have developed a technique, called ASA-PD (Advanced Sensing of Aggregates for Parkinson’s Disease), which uses ultra-sensitive fluorescence microscopy to detect and analyze millions of oligomers in post-mortem brain tissue. Since oligomers are so small, their signal is extremely weak. ASA-PD maximizes the signal while decreasing the background, dramatically boosting sensitivity to the point where individual alpha-synuclein oligomers can be observed and studied.
“This is the first time we’ve been able to look at oligomers directly in human brain tissue at this scale: it’s like being able to see stars in broad daylight,” said co-first author Dr Rebecca Andrews, who conducted the work when she was a postdoctoral researcher in Lee’s lab. “It opens new doors in Parkinson’s research.”
Uncovering the Earliest Markers of Disease
The team examined post-mortem brain tissue samples from people with Parkinson’s and compared them to healthy individuals of similar age. They found that oligomers exist in both healthy and Parkinson’s brains. The main difference between disease and healthy brains was the size of the oligomers, which were larger, brighter, and more numerous in disease samples, suggesting a direct link to the progression of Parkinson’s.
The team also discovered a subclass of oligomers that appeared only in Parkinson’s patients, which could be the earliest visible markers of the disease – potentially years before symptoms appear.
“This method doesn’t just give us a snapshot,” said Professor Lucien Weiss from Polytechnique Montréal, wo co-led the research. “It offers a whole atlas of protein changes across the brain and similar technologies could be applied to other neurodegenerative diseases like Alzheimer’s and Huntington’s.
“Oligomers have been the needle in the haystack, but now that we know where those needles are, it could help us target specific cell types in certain regions of the brain.”
“The only real way to understand what is happening in human disease is to study the human brain directly, but because of the brain’s sheer complexity, this is very challenging,” said Professor Sonia Gandhi from The Francis Crick Institute, who co-led the research. “We hope that breaking through this technological barrier will allow us to understand why, where, and how protein clusters form and how this changes the brain environment and leads to disease.”
Reference: “Large-scale visualization of α-synuclein oligomers in Parkinson’s disease brain tissue” by Rebecca Andrews, Bin Fu, Christina E. Toomey, Jonathan C. Breiter, Joanne Lachica, Joseph S. Beckwith, Ru Tian, Emma E. Brock, Lisa-Maria Needham, Gregory J. Chant, Camille Loiseau, Angèle Deconfin, Kenza Baspin, Rebeka Popovic, James Evans, Yen Goh, Begüm Kurt, Lenart Senicar, Marisa Edmonds, Tim Bartels, Nora Bengoa-Vergniory, Peter J. Magill, Zane Jaunmuktane, Oliver J. Freeman, Benjamin J. M. Taylor, John Hardy, Tammaryn Lashley, Mina Ryten, Michele Vendruscolo, Nicholas W. Wood, Lucien E. Weiss, Sonia Gandhi and Steven F. Lee, 31 September 2025, Nature Biomedical Engineering.
DOI: 10.1038/s41551-025-01496-4
The research was supported in part by Aligning Science Across Parkinson’s (ASAP), the Michael J. Fox Foundation, and the Medical Research Council (MRC), part of UK Research and Innovation (UKRI). The researchers thank the patients, families and carers who donated tissue to brain banks to enable this work to happen.
Never miss a breakthrough: Join the SciTechDaily newsletter.
Follow us on Google, Discover, and News.
Get the source article here