As Parkinson’s progresses, ‘off’ periods can become more common – so how can people with the condition respond when these states occur? Neurologist Dr Werner Poewe and Dr Sara Riggare, a researcher living with the condition, share their perspectives on managing ‘off’ periods and discuss the solutions available
Dr Sara Riggare first experienced Parkinson’s symptoms when she was only 13 years old – but she didn’t receive a diagnosis until nearly two decades later, at the age of 32. “It was a pretty hard blow,” she admits.
Since then, the Sweden-based researcher and former engineer has used her experience to further understanding of the condition. She recently completed her doctorate, in which her thesis focused on Parkinson’s and patient-led research. “I’ve tried to help myself and others living with chronic conditions – I want to bring researchers and people with these conditions closer together,” she explains.
For Sara and other people with Parkinson’s, living with the condition means having to deal with ‘off’ periods – when symptoms return as a result of medication not working the way it should.
“There is a spectrum of problems than can occur during ‘off’ periods,” says Dr Werner Poewe, director of neurology at Innsbruck Medical University, Austria – whose brother was diagnosed with the condition a few years ago.
“There are a lot of things people can do to reduce ‘off’ periods,” he explains. “Number one is recognising the problem. That may sound straightforward, but it’s not. For any healthcare provider, this is about working out when problems tend to occur and trying to recognise the pattern.”
Sara, for example, finds that her symptoms are worse when she wakes up in the morning. “Everything takes much more effort,” she says. “I’m clumsier, I’m slower, I’m sluggish. I have to focus really hard to move.”
Tackling ‘off’ periods was initially a challenge for her. “It’s difficult to know what to expect until you’ve had them yourself,” she says. “It was surprising to me at first, how all-encompassing they are – both on the body and the brain.” But as her condition has progressed, Sara has found ways to manage these ‘off’ states.
A holistic approach to addressing ‘off’ periods
Both Werner and Sara agree that it’s important to practice habits that reduce the frequency of ‘off’ periods. “It’s about having a balanced life in terms of stress, sleep, activity, diet,” says Sara. “Basically, what is good for everybody is especially important for people with Parkinson’s.”
She also carefully times her medication intake to prevent the effects from wearing off and causing her Parkinson’s symptoms to flare up again: “Managing my medications and optimising their impact has helped make my ‘off’ periods less severe.”

Sara and Werner agree that carefully timing medication intake may help with ‘off’ period management.
Werner emphasises the importance of scheduling levodopa intake to limit fluctuations, and ensuring that this medication is combined with specific enzyme inhibitors – which work to prevent the breakdown of levodopa before it reaches the brain – and dopamine agonists that mimic the way the dopamine chemical works.
“In the early stages of the condition, I usually recommend that people take their doses of levodopa (a common Parkinson’s medication) four hours apart,” he says. “After that point, most of the drug is cleared from the circulation.”
The pair agree that each individual must explore which management options are best suited for them. “Understand your own ‘off’ periods as well as you can,” says Sara. “Are they caused by medication? Are they caused by something external? Try to read up about potential explanations.”
“It’s all about someone with Parkinson’s being able to decide for themselves what is the right way forward,” adds Werner.
Turning to on-demand remedies
While there are measures that people can take to try to prevent ‘off’ periods, including taking notes on warning signs and carefully timing medication intake, Werner notes: “People with Parkinson’s may have done everything they can and still get periods from time to time when they’re not switching ‘on’.”
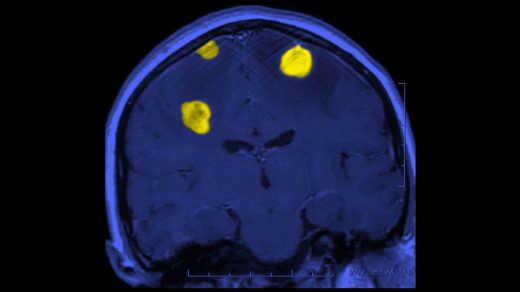
For people who experience intermittent ‘off’ states – from partial or complete medication failure to unpredictable ‘offs’ – fast-acting remedies may be beneficial.
These on-demand therapies come in various forms, all designed to help stop ‘off’ periods in their tracks. Fast-acting versions of levodopa, for example, can be inhaled or mixed with water for drinking. Different forms of apomorphine, a type of dopamine agonist, may also provide relief – whether placed under the tongue or injected into the skin.
As Werner notes: “These on-demand treatments can be very beneficial, because they work rapidly to get people out of unpleasant situations.”
But, as with all medications, it’s important to consider potential drawbacks and side effects. “Some people don’t like to inject themselves with a subcutaneous (under the skin) device,” says Werner. “Others may be irritative to sublingual (under the tongue) treatment – there might be reddening, pain or even little ulcers in the mouth. Some people who inhale levodopa, meanwhile, complain about feeling the need to cough.”
The variety of available therapies can help people with Parkinson’s tailor treatment to their preferences – and better supplement their everyday fixed medication regimen.
While Werner says it’s important for people with the condition to “be prepared and have on-demand strategies in place” in case an unexpected situation arises, he also emphasises that there is no one-size-fits-all approach to managing ‘off’ periods.
Sara agrees, saying: “Do not put all of your eggs in one basket.”
Lead image: Dr Sara Riggare, photographed by Helena Conning.
This article is sponsored by Bial, a pharmaceutical company committed to discovering, developing and commercialising medicines with the aim of improving people’s lives worldwide.
For more information on Parkinson’s therapies, visit the Parkinson’s Europe website.
Read more:
What are ‘off’ periods – and how can they impact people with Parkinson’s disease?
How can people with Parkinson’s disease recognise and anticipate ‘off’ periods?