A new support group at the UT Health San Antonio Center for Brain Health is giving patients with Parkinson’s disease a rare opportunity: to learn directly from other patients who have already undergone deep brain stimulation (DBS), a surgical treatment that can significantly improve quality of life but remains widely underused.
Deep brain stimulation has been approved for essential tremor since 1997 and for Parkinson’s disease since 2002. Despite more than two decades of proven effectiveness, only about 10% of Parkinson’s patients ultimately choose to undergo the procedure. According to Okeanis Vaou, MD, FAAN, fear and lack of understanding are the major barriers.

“Deep brain stimulation is often perceived as frightening because people hear the words ‘brain surgery’ and stop there,” said Vaou, chief of the Movement Disorders Division at The University of Texas at San Antonio and neurologist at UT Health San Antonio, the academic health center of UT San Antonio. “But it’s a minimally invasive procedure with very low risk, especially when performed by experienced surgeons. For many patients, it can be life changing.”
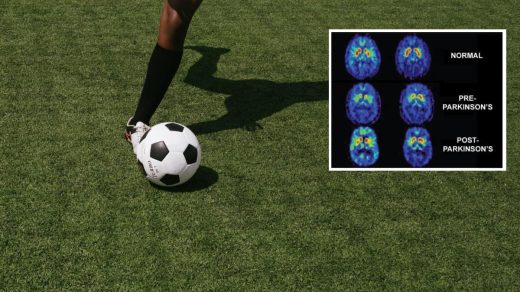
The procedure works by delivering continuous electrical stimulation to specific areas of the brain responsible for tremor, rigidity and slowed movement. It is typically recommended when medications are no longer sufficient to control motor symptoms. When used alongside medication, DBS can provide years of improved symptom control and enhanced quality of life.
Vaou created the DBS support group with Kristen Matulis, DNP, APRN, AGNP-C, an adult and gerontology nurse practitioner specializing in movement disorders at UT Health San Antonio. Their aim for the group was to bring together patients who are considering DBS with those who have already had the procedure. The monthly support group is designed to address the emotional and informational gap that often exists when DBS is first introduced as a treatment option.
The program officially launched its first cohort on Jan.15, drawing 24 patients and care partners — a high early turnout that demonstrates a major unmet need.

“We were incredibly excited by the turnout because it clearly showed the need for something like this for patients. They are really seeking education from and connection with others who have already undergone DBS and those who are currently in the evaluation process,” Matulis said. “Based on the feedback from the first session, several preoperative patients expressed how helpful it was to meet individuals and care partners who had experienced similar symptoms and could speak firsthand about how DBS helped them.”
Matulis also emphasized the value of shared experience not only for patients, but for caregivers as well.
“Hearing how DBS affected someone’s daily life, independence and overall well-being makes a real difference,” she said. “It’s also meaningful for care partners to understand how caregiver burden can change after surgery.”
In addition to its support-focused mission, the group has a research component. The team plans to collect data on caregiver burden before and after DBS to better understand whether the procedure has a measurable impact on those providing care — an area that has received less attention in clinical research.
The group meets monthly in the multipurpose room at the Center for Brain Health, a setting chosen intentionally for its holistic, multidisciplinary approach to neurological care. Vaou and Matulis hope the support group program, a first of its kind in San Antonio, will continue to grow and reach patients across the region and serve as a model for similar initiatives elsewhere.
“Our goal is also to reach under-resourced populations in San Antonio and South Texas. We want to grow this program so that people who may not have access to movement disorder specialists in their hometowns, who may have to travel long distances for care, can still receive this education and support,” Matulis said.
As interest continues to build, the team hopes the support group will not only improve decision-making around DBS but also help redefine how advanced Parkinson’s care is delivered through education, community and shared understanding.
“We want to help empower patients with knowledge, connection and real-life perspective,” Vaou said. “That patient-to-patient connection is incredibly powerful and something that’s rarely built into traditional care models.”